Page 191 - Critical Care Notes
P. 191
4223_Tab06_175-198 29/08/14 8:27 AM Page 185
185
■ Grade 3: Somnolence to semistupor, response to verbal stimuli,
confusion
■ Grade 4: Coma, lack of response to stimuli
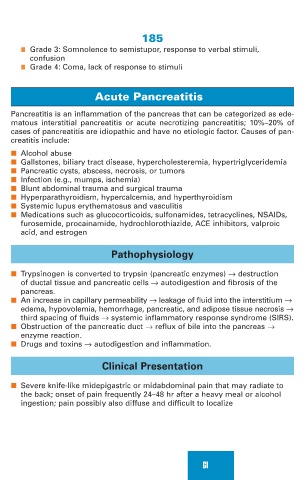
Acute Pancreatitis
Pancreatitis is an inflammation of the pancreas that can be categorized as ede-
matous interstitial pancreatitis or acute necrotizing pancreatitis; 10%–20% of
cases of pancreatitis are idiopathic and have no etiologic factor. Causes of pan-
creatitis include:
■ Alcohol abuse
■ Gallstones, biliary tract disease, hypercholesteremia, hypertriglyceridemia
■ Pancreatic cysts, abscess, necrosis, or tumors
■ Infection (e.g., mumps, ischemia)
■ Blunt abdominal trauma and surgical trauma
■ Hyperparathyroidism, hypercalcemia, and hyperthyroidism
■ Systemic lupus erythematosus and vasculitis
■ Medications such as glucocorticoids, sulfonamides, tetracyclines, NSAIDs,
furosemide, procainamide, hydrochlorothiazide, ACE inhibitors, valproic
acid, and estrogen
Pathophysiology
■ Trypsinogen is converted to trypsin (pancreatic enzymes) → destruction
of ductal tissue and pancreatic cells → autodigestion and fibrosis of the
pancreas.
■ An increase in capillary permeability → leakage of fluid into the interstitium →
edema, hypovolemia, hemorrhage, pancreatic, and adipose tissue necrosis →
third spacing of fluids → systemic inflammatory response syndrome (SIRS).
■ Obstruction of the pancreatic duct → reflux of bile into the pancreas →
enzyme reaction.
■ Drugs and toxins → autodigestion and inflammation.
Clinical Presentation
■ Severe knife-like midepigastric or midabdominal pain that may radiate to
the back; onset of pain frequently 24–48 hr after a heavy meal or alcohol
ingestion; pain possibly also diffuse and difficult to localize
GI