Page 77 - Critical Care Notes
P. 77
4223_Tab02_045-106 29/08/14 10:00 AM Page 71
71
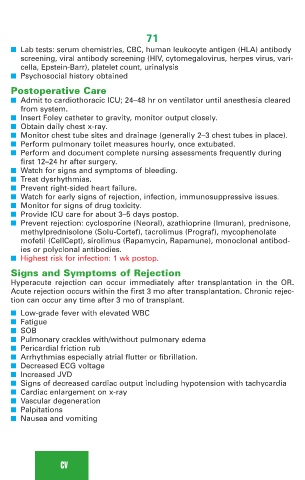
■ Lab tests: serum chemistries, CBC, human leukocyte antigen (HLA) antibody
screening, viral antibody screening (HIV, cytomegalovirus, herpes virus, vari-
cella, Epstein-Barr), platelet count, urinalysis
■ Psychosocial history obtained
Postoperative Care
■ Admit to cardiothoracic ICU; 24–48 hr on ventilator until anesthesia cleared
from system.
■ Insert Foley catheter to gravity, monitor output closely.
■ Obtain daily chest x-ray.
■ Monitor chest tube sites and drainage (generally 2–3 chest tubes in place).
■ Perform pulmonary toilet measures hourly, once extubated.
■ Perform and document complete nursing assessments frequently during
first 12–24 hr after surgery.
■ Watch for signs and symptoms of bleeding.
■ Treat dysrhythmias.
■ Prevent right-sided heart failure.
■ Watch for early signs of rejection, infection, immunosuppressive issues.
■ Monitor for signs of drug toxicity.
■ Provide ICU care for about 3–5 days postop.
■ Prevent rejection: cyclosporine (Neoral), azathioprine (Imuran), prednisone,
methylprednisolone (Solu-Cortef), tacrolimus (Prograf), mycophenolate
mofetil (CellCept), sirolimus (Rapamycin, Rapamune), monoclonal antibod-
ies or polyclonal antibodies.
■ Highest risk for infection: 1 wk postop.
Signs and Symptoms of Rejection
Hyperacute rejection can occur immediately after transplantation in the OR.
Acute rejection occurs within the first 3 mo after transplantation. Chronic rejec-
tion can occur any time after 3 mo of transplant.
■ Low-grade fever with elevated WBC
■ Fatigue
■ SOB
■ Pulmonary crackles with/without pulmonary edema
■ Pericardial friction rub
■ Arrhythmias especially atrial flutter or fibrillation.
■ Decreased ECG voltage
■ Increased JVD
■ Signs of decreased cardiac output including hypotension with tachycardia
■ Cardiac enlargement on x-ray
■ Vascular degeneration
■ Palpitations
■ Nausea and vomiting
CV