Page 2497 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 2497
Chapter 152 Hematologic Manifestations of Childhood Illness 2229
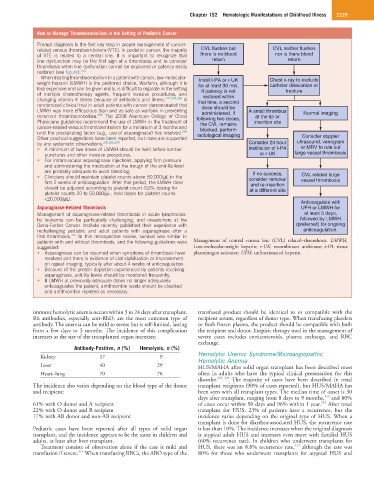
How to Manage Thromboembolism in the Setting of Pediatric Cancer
Prompt diagnosis is the first key step in proper management of cancer-
related venous thromboembolism (VTE). In pediatric cancer, the majority CVL flushes but CVL neither flushes
of VTE is related to a central line. It is important to recognize that there is no blood nor is there blood
line dysfunction may be the first sign of a thrombosis and to consider return return
thrombosis when line dysfunction cannot be explained or patency easily
restored (see figure). 254
When treating thromboembolism in a patient with cancer, low-molecular- Instill t-PA or r-UK Chest x-ray to exclude
weight heparin (LMWH) is the preferred choice. Warfarin, although it is for at least 30 min. catheter dislocation or
less expensive and can be given orally, is difficult to regulate in the setting If patency is not fracture
of multiple chemotherapy agents, frequent invasive procedures, and restored within
changing vitamin K stores because of antibiotics and illness. 247,304,305 A that time, a second
randomized clinical trial in adult patients with cancer demonstrated that dose should be
LMWH was more efficacious than and as safe as warfarin in preventing administered. If A small thrombus Normal imaging
recurrent thromboembolism. 306 The 2008 American College of Chest following two doses, at the tip or
Physicians guidelines recommend the use of LMWH in the treatment of the CVL remains insertion site
cancer-related venous thromboembolism for a minimum of 3 months and blocked, perform
until the precipitating factor (e.g., use of asparaginase) has resolved. 286 radiological imaging
Other practical suggestions have been reported, but none are supported Consider doppler
by any systematic observations. 260,286,304 Consider 24 hour ultrasound, venogram
• A minimum of two doses of LMWH should be held before lumbar instillation of t-PA or MRV to rule out
punctures and other invasive procedures. or r-UK large vessel thrombosis
• For intramuscular asparaginase injections, applying firm pressure
and administering the medication at the trough of the anti-Xa level
are probably adequate to avoid bleeding. If no success,
• Clinicians should maintain platelet counts above 50,000/µL in the consider removal CVL related large
first 2 weeks of anticoagulation. After that period, the LMWH dose and re-insertion vessel thrombosis
should be adjusted according to platelet count (50% dosing for at a different site
platelet counts 20 to 50,000/µL; hold doses for platelet counts
<20,000/µL).
Anticoagulate with
Asparaginase-Related Thrombosis UFH or LMWH for
Management of asparaginase-related thrombosis in acute lymphoblas- at least 5 days,
tic leukemia can be particularly challenging, and researchers at the followed by LMWH
Dana-Farber Cancer Institute recently published their experience with (preferred) for ongoing
rechallenging pediatric and adult patients with asparaginase after a anticoagulation.
first thrombosis. 307 In this retrospective review, survival was similar in
patients with and without thrombosis, and the following guidelines were Management of central venous line (CVL) related–thrombosis. LMWH,
suggested: Low-molecular-weight heparin; r-UK, recombinant urokinase; t-PA, tissue
• Asparaginase can be resumed when symptoms of thrombosis have plasminogen activator; UFH, unfractionated heparin.
resolved and there is evidence of clot stabilization or improvement
on repeat imaging, typically after about 4 weeks of anticoagulation.
• Because of the protein depletion experienced by patients receiving
asparaginase, anti-Xa levels should be monitored frequently.
• If LMWH at previously adequate doses no longer adequately
anticoagulates the patient, antithrombin levels should be checked
and antithrombin repleted as necessary.
immune hemolytic anemia occurs within 3 to 24 days after transplant. transfused product should be identical to or compatible with the
Rh antibodies, especially anti-RhD, are the most common type of recipient serum, regardless of donor type. When transfusing platelets
antibody. The anemia can be mild to severe but is self-limited, lasting or fresh frozen plasma, the product should be compatible with both
from a few days to 3 months. The incidence of this complication the recipient and donor. Empiric therapy used in the management of
increases as the size of the transplanted organ increases: severe cases includes corticosteroids, plasma exchange, and RBC
exchange.
Antibody-Positive, n (%) Hemolysis, n (%)
Kidney 17 9 Hemolytic Uremic Syndrome/Microangiopathic
Hemolytic Anemia
Liver 40 29 HUS/MAHA after solid organ transplant has been described most
Heart–lung 70 70 often in adults who have the typical clinical presentation for this
disorder. 322–324 The majority of cases have been described in renal
The incidence also varies depending on the blood type of the donor transplant recipients (90% of cases reported), but HUS/MAHA has
and recipient: been seen with all transplant types. The median time of onset is 30
322
days after transplant, ranging from 8 days to 9 months, and 80%
324
61% with O donor and A recipient of cases occur within 90 days and 96% within 1 year. After renal
22% with O donor and B recipient transplant for HUS, 23% of patients have a recurrence, but the
17% with AB donor and non-AB recipient incidence varies depending on the original type of HUS. When a
transplant is done for diarrhea-associated HUS, the recurrence rate
Pediatric cases have been reported after all types of solid organ is less than 10%. The incidence increases when the original diagnosis
transplant, and the incidence appears to be the same in children and is atypical adult HUS and increases even more with familial HUS
adults, at least after liver transplant. (60% recurrence rate). In children who underwent transplants for
323
Treatment consists of observation alone if the case is mild and HUS, there was an 8.8% recurrence rate, although the rate was
319
transfusion if severe. When transfusing RBCs, the ABO type of the 80% for those who underwent transplants for atypical HUS and