Page 13 - SC4Q-2019-
P. 13
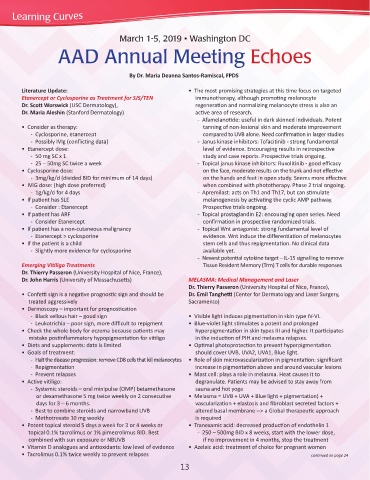
March 1-5, 2019 • Washington DC
AAD Annual Meeting Echoes
By Dr. Maria Deanna Santos-Ramiscal, FPDS
Literature Update: • The most promising strategies at this time focus on targeted
Etanercept or Cyclosporine as Treatment for SJS/TEN immunotherapy, although promoting melanocyte
Dr. Scott Worswick (USC Dermatology), regeneration and normalizing melanocyte stress is also an
Dr. Maria Aleshin (Stanford Dermatology) active area of research.
- Afamelanotide: useful in dark skinned individuals. Potent
• Consider as therapy: tanning of non-lesional skin and moderate improvement
- Cyclosporine, etanercept compared to UVB alone. Need confirmation in larger studies
- Possibly IVIg (conflicting data) - Janus kinase inhibitors: Tofacitinib - strong fundamental
• Etanercept dose: level of evidence. Encouraging results in retrospective
- 50 mg SC x 1 study and case reports. Prospective trials ongoing.
- 25 – 50mg SC twice a week - Topical janus kinase inhibitors: Ruxolitinib - good efficacy
• Cyclosporine dose: on the face, moderate results on the trunk and not effective
- 3mg/kg/d (divided BID for minimum of 14 days) on the hands and feet in open study. Seems more effective
• IVIG dose: (high dose preferred) when combined with phototherapy. Phase 2 trial ongoing.
- 1g/kg/d for 4 days - Apremilast: acts on Th1 and Th17, but can stimulate
• If patient has SLE melanogenesis by activating the cyclic AMP pathway.
- Consider : Etanercept Prospective trials ongoing.
• If patient has ARF - Topical prostaglandin E2: encouraging open series. Need
- Consider Etanercept confirmation in prospective randomized trials.
• If patient has a non-cutaneous malignancy - Topical Wnt antagonist: strong fundamental level of
- Etanercept > cyclosporine evidence. Wnt induce the differentiation of melanocytes
• If the patient is a child stem cells and thus repigmentation. No clinical data
- Slightly more evidence for cyclosporine available yet.
- Newest potential cytokine target – IL-15 signalling to remove
Emerging Vitiligo Treatments Tissue Resident Memory (Trm) T cells for durable responses
Dr. Thierry Passeron (University Hospital of Nice, France),
Dr. John Harris (University of Massachusetts) MELASMA: Medical Management and Laser
Dr. Thierry Passeron (University Hospital of Nice, France),
• Confetti sign is a negative prognostic sign and should be Dr. Emil Tanghetti (Center for Dermatology and Laser Surgery,
treated aggressively Sacramento)
• Dermoscopy – important for prognostication
- Black vellous hair – good sign • Visible light induces pigmentation in skin type IV-VI.
- Leukotrichia – poor sign, more difficult to repigment • Blue-violet light stimulates a potent and prolonged
• Check the whole body for eczema because patients may hyperpigmentation in skin types III and higher. It participates
mistake postinflammatory hypopigmentation for vitiligo in the induction of PIH and melasma relapses.
• Diets and supplements: data is limited • Optimal photoprotection to prevent hyperpigmentation
• Goals of treatment: should cover UVB, UVA2, UVA1, Blue light.
- Halt the disease progression: remove CD8 cells that kill melanocytes • Role of skin microvascularization in pigmentation: significant
- Repigmentation increase in pigmentation above and around vascular lesions
- Prevent relapses • Mast cell: plays a role in melasma. Heat causes it to
• Active vitiligo: degranulate. Patients may be advised to stay away from
- Systemic steroids – oral minipulse (OMP) betamethasone sauna and hot yoga
or dexamethasone 5 mg twice weekly on 2 consecutive • Melasma = UVB + UVA + Blue light + pigmentation) +
days for 3 – 6 months. vascularization + elastosis and fibroblast secreted factors +
- Best to combine steroids and narrowband UVB altered basal membrane --> a Global therapeutic approach
- Methotrexate 10 mg weekly is required
• Potent topical steroid 5 days a week for 3 or 4 weeks or • Tranexamic acid: decreased production of endothelin 1
topical 0.1% tacrolimus or 1% pimecrolimus BID. Best - 250 – 500mg BID x 8 weeks, start with the lower dose,
combined with sun exposure or NBUVB if no improvement in 4 months, stop the treatment
• Vitamin D analogues and antioxidants: low level of evidence • Azelaic acid: treatment of choice for pregnant women
• Tacrolimus 0.1% twice weekly to prevent relapses continued on page 14
13