Page 813 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 813
544 PART 5: Infectious Disorders
CHAPTER Principles of Antimicrobial a low V and therefore are greatly affected by these fluid shifts. Since
d
lipophilic antimicrobials have a larger V , they typically distribute further
d
61 Therapy and the Clinical into tissues and are less affected by these fluid shifts. Patients in the
ICU often have hypotension as a result of septic shock, which requires
Pharmacology of the administration of fluid boluses. Additionally, heart failure and renal
Antimicrobial Drugs failure lead to more edematous states where patients can retain large
amounts of fluid. These situations also lead to increases in V of hydro-
d
philic drugs. Changes in protein binding can also have a substantial
Amira Ashok Bhalodi effect on the V , especially for drugs that are highly protein bound. Only
David P. Nicolau d
unbound or free drug is microbiologically active. Hypoalbuminemia
in critically ill patients can result in decreased binding of drugs and
subsequently higher free concentrations of drugs. While free drug will
KEY POINTS
distribute into tissues, critically ill patients often have greater amounts
• The altered pharmacokinetics of critically ill patients can greatly of fluid in the interstitial space causing the antimicrobial concentrations
impact antimicrobial exposures. Recognizing these changes and in the tissues to remain low. 3
optimizing antimicrobial administration to make certain appro- The administration of large volumes of fluid and use of vasopressors
priate pharmacodynamic targets are reached is crucial in ensuring leads to a hypermetabolic state in which cardiac output and glomerular
successful outcomes. filtration rate are increased. It has been shown in animal studies that
• Understanding the impact of the MIC of the pathogen on overall increases in cardiac output result in increases in renal blood flow. The
free-drug exposures is important to be able to reach required term often used to describe this enhanced elimination is augmented
4
pharmacodynamic targets of efficacy. Ultimately, organisms with renal clearance. These physiological changes affect the clearance of
high MICs will require a larger free-drug exposure compared with drugs and can lead to subtherapeutic levels of antimicrobials that
organisms with lower MICs. are typically cleared renally. In contrast, decreased organ perfusion
• Patients with augmented renal function will exhibit enhanced clear- in the presence of end organ damage can lead to kidney and/or liver
failure in which concentrations of these antimicrobials would be
ance of antimicrobials, particularly β-lactams, and are at risk for increased. Inadequate clearance or metabolism of these drugs would
subtherapeutic exposures. Therefore, these patients often require lead to accumulation and potential toxicity. Typically, equations such
higher doses and more frequent administration of the antimicrobial. as Cockroft-Gault are used to estimate renal function; however, these
• Antimicrobial stewardship focused on disease state management are often not good predictors of renal function in critically ill patients
and selecting the appropriate antimicrobial therapy for the infect- due to the acute and rapid changes such patients often experience. Since
ing pathogen is essential in preventing poor outcomes. In addition many antimicrobials are dosed based on renal function it is even more
to poor outcomes, failure to treat infections appropriately can lead challenging to ensure adequate doses are being administered. The most
to the emergence of resistant organisms that become increasingly accurate way to calculate renal function is the use of 8- or 12-hour
difficult to treat. creatinine collections. In situations where renal replacement therapy
2
• Given the vast majority of antimicrobials are renally cleared, is utilized, careful consideration of timing and supplemental dosing
concentrations of antimicrobials are affected by continuous renal post-dialysis would be needed depending on the antimicrobial agent.
replacement therapy and therefore dosing should be modified Understanding the pharmacokinetics factors that affect drug con-
accordingly to obtain adequate target exposures. centrations is essential in ensuring drugs are delivered to the target
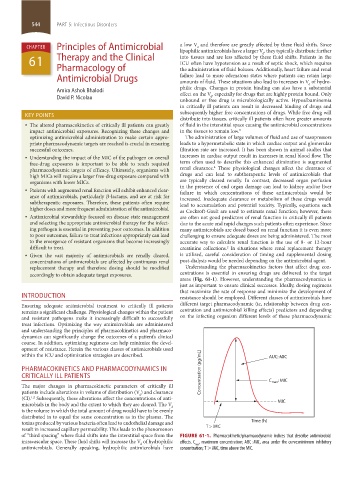
areas (Fig. 61-1). However, understanding the pharmacodynamics is
just as important to ensure clinical successes. Ideally, dosing regimens
that maximize the rate of response and minimize the development of
INTRODUCTION resistance should be employed. Different classes of antimicrobials have
Ensuring adequate antimicrobial treatment to critically ill patients different target pharmacodynamic (ie, relationship between drug con-
remains a significant challenge. Physiological changes within the patient centration and antimicrobial killing effects) predictors and depending
and resistant pathogens make it increasingly difficult to successfully on the infecting organism different levels of these pharmacodynamic
treat infections. Optimizing the way antimicrobials are administered
and understanding the principles of pharmacokinetics and pharmaco-
dynamics can significantly change the outcomes of a patient’s clinical
course. In addition, optimizing regimens can help minimize the devel-
opment of resistance. Herein the various classes of antimicrobials used
within the ICU and optimization strategies are described. AUC: MIC
PHARMACOKINETICS AND PHARMACODYNAMICS IN
CRITICALLY ILL PATIENTS Concentration ( g/mL) C : MIC
The major changes in pharmacokinetic parameters of critically ill max
patients include alterations in volume of distribution (V ) and clearance
d
(Cl). Subsequently, these alterations affect the concentrations of anti-
1,2
microbials in the body and the extent to which they are cleared. The V MIC
d
is the volume in which the total amount of drug would have to be evenly
distributed in to equal the same concentration as in the plasma. The
toxins produced by various bacteria often lead to endothelial damage and Time (h)
result in increased capillary permeability. This leads to the phenomenon T > MIC
of “third spacing” where fluid shifts into the interstitial space from the FIGURE 61-1. Pharmacokinetic/pharmacodynamic indices that describe antimicrobial
intravascular space. These fluid shifts will increase the V of hydrophilic effects. C , maximum concentration; AUC : MIC, area under the curve:minimum inhibitory
d
max
antimicrobials. Generally speaking, hydrophilic antimicrobials have concentration; T > MIC, time above the MIC.
section05_c61-73.indd 544 1/23/2015 12:47:12 PM