Page 172 - Critical Care Notes
P. 172
4223_Tab05_141-174 29/08/14 8:28 AM Page 166
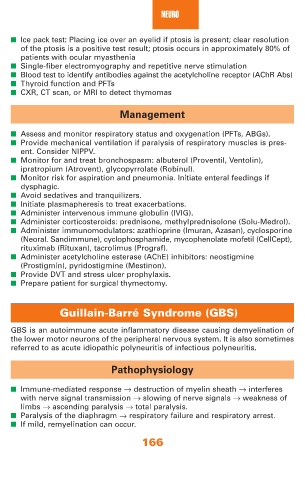
NEURO
■ Ice pack test: Placing ice over an eyelid if ptosis is present; clear resolution
of the ptosis is a positive test result; ptosis occurs in approximately 80% of
patients with ocular myasthenia
■ Single-fiber electromyography and repetitive nerve stimulation
■ Blood test to identify antibodies against the acetylcholine receptor (AChR Abs)
■ Thyroid function and PFTs
■ CXR, CT scan, or MRI to detect thymomas
Management
■ Assess and monitor respiratory status and oxygenation (PFTs, ABGs).
■ Provide mechanical ventilation if paralysis of respiratory muscles is pres-
ent. Consider NIPPV.
■ Monitor for and treat bronchospasm: albuterol (Proventil, Ventolin),
ipratropium (Atrovent), glycopyrrolate (Robinul).
■ Monitor risk for aspiration and pneumonia. Initiate enteral feedings if
dysphagic.
■ Avoid sedatives and tranquilizers.
■ Initiate plasmapheresis to treat exacerbations.
■ Administer intervenous immune globulin (IVIG).
■ Administer corticosteroids: prednisone, methylprednisolone (Solu-Medrol).
■ Administer immunomodulators: azathioprine (Imuran, Azasan), cyclosporine
(Neoral. Sandimmune), cyclophosphamide, mycophenolate mofetil (CellCept),
rituximab (Rituxan), tacrolimus (Prograf).
■ Administer acetylcholine esterase (AChE) inhibitors: neostigmine
(Prostigmin), pyridostigmine (Mestinon).
■ Provide DVT and stress ulcer prophylaxis.
■ Prepare patient for surgical thymectomy.
Guillain-Barré Syndrome (GBS)
GBS is an autoimmune acute inflammatory disease causing demyelination of
the lower motor neurons of the peripheral nervous system. It is also sometimes
referred to as acute idiopathic polyneuritis of infectious polyneuritis.
Pathophysiology
■ Immune-mediated response → destruction of myelin sheath → interferes
with nerve signal transmission → slowing of nerve signals → weakness of
limbs → ascending paralysis → total paralysis.
■ Paralysis of the diaphragm → respiratory failure and respiratory arrest.
■ If mild, remyelination can occur.
166