Page 168 - Critical Care Notes
P. 168
4223_Tab05_141-174 29/08/14 8:28 AM Page 162
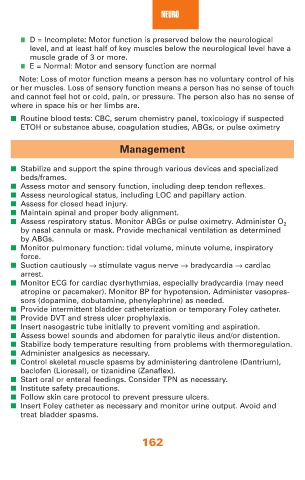
NEURO
■ D = Incomplete: Motor function is preserved below the neurological
level, and at least half of key muscles below the neurological level have a
muscle grade of 3 or more.
■ E = Normal: Motor and sensory function are normal
Note: Loss of motor function means a person has no voluntary control of his
or her muscles. Loss of sensory function means a person has no sense of touch
and cannot feel hot or cold, pain, or pressure. The person also has no sense of
where in space his or her limbs are.
■ Routine blood tests: CBC, serum chemistry panel, toxicology if suspected
ETOH or substance abuse, coagulation studies, ABGs, or pulse oximetry
Management
■ Stabilize and support the spine through various devices and specialized
beds/frames.
■ Assess motor and sensory function, including deep tendon reflexes.
■ Assess neurological status, including LOC and papillary action.
■ Assess for closed head injury.
■ Maintain spinal and proper body alignment.
■ Assess respiratory status. Monitor ABGs or pulse oximetry. Administer O 2
by nasal cannula or mask. Provide mechanical ventilation as determined
by ABGs.
■ Monitor pulmonary function: tidal volume, minute volume, inspiratory
force.
■ Suction cautiously → stimulate vagus nerve → bradycardia → cardiac
arrest.
■ Monitor ECG for cardiac dysrhythmias, especially bradycardia (may need
atropine or pacemaker). Monitor BP for hypotension. Administer vasopres-
sors (dopamine, dobutamine, phenylephrine) as needed.
■ Provide intermittent bladder catheterization or temporary Foley catheter.
■ Provide DVT and stress ulcer prophylaxis.
■ Insert nasogastric tube initially to prevent vomiting and aspiration.
■ Assess bowel sounds and abdomen for paralytic ileus and/or distention.
■ Stabilize body temperature resulting from problems with thermoregulation.
■ Administer analgesics as necessary.
■ Control skeletal muscle spasms by administering dantrolene (Dantrium),
baclofen (Lioresal), or tizanidine (Zanaflex).
■ Start oral or enteral feedings. Consider TPN as necessary.
■ Institute safety precautions.
■ Follow skin care protocol to prevent pressure ulcers.
■ Insert Foley catheter as necessary and monitor urine output. Avoid and
treat bladder spasms.
162