Page 201 - Critical Care Notes
P. 201
4223_Tab06_175-198 29/08/14 8:27 AM Page 195
195
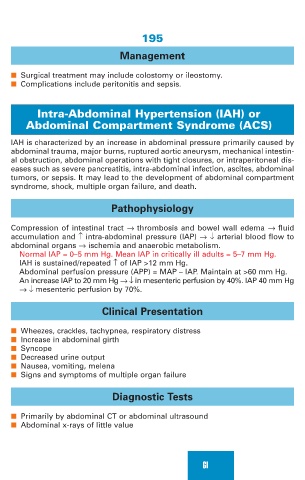
Management
■ Surgical treatment may include colostomy or ileostomy.
■ Complications include peritonitis and sepsis.
Intra-Abdominal Hypertension (IAH) or
Abdominal Compartment Syndrome (ACS)
IAH is characterized by an increase in abdominal pressure primarily caused by
abdominal trauma, major burns, ruptured aortic aneurysm, mechanical intestin-
al obstruction, abdominal operations with tight closures, or intraperitoneal dis-
eases such as severe pancreatitis, intra-abdominal infection, ascites, abdominal
tumors, or sepsis. It may lead to the development of abdominal compartment
syndrome, shock, multiple organ failure, and death.
Pathophysiology
Compression of intestinal tract → thrombosis and bowel wall edema → fluid
accumulation and ↑ intra-abdominal pressure (IAP) →↓ arterial blood flow to
abdominal organs → ischemia and anaerobic metabolism.
Normal IAP = 0–5 mm Hg. Mean IAP in critically ill adults = 5–7 mm Hg.
IAH is sustained/repeated ↑ of IAP >12 mm Hg.
Abdominal perfusion pressure (APP) = MAP – IAP. Maintain at >60 mm Hg.
An increase IAP to 20 mm Hg → ↓ in mesenteric perfusion by 40%. IAP 40 mm Hg
→ ↓ mesenteric perfusion by 70%.
Clinical Presentation
■ Wheezes, crackles, tachypnea, respiratory distress
■ Increase in abdominal girth
■ Syncope
■ Decreased urine output
■ Nausea, vomiting, melena
■ Signs and symptoms of multiple organ failure
Diagnostic Tests
■ Primarily by abdominal CT or abdominal ultrasound
■ Abdominal x-rays of little value
GI