Page 222 - Critical Care Notes
P. 222
4223_Tab08_216-229 29/08/14 8:26 AM Page 216
ENDO
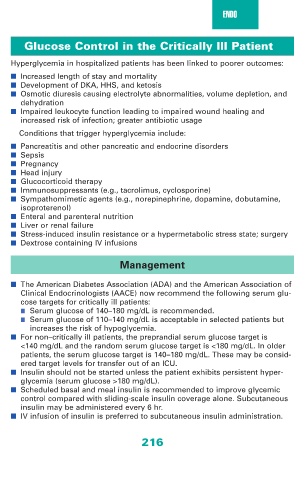
Glucose Control in the Critically Ill Patient
Hyperglycemia in hospitalized patients has been linked to poorer outcomes:
■ Increased length of stay and mortality
■ Development of DKA, HHS, and ketosis
■ Osmotic diuresis causing electrolyte abnormalities, volume depletion, and
dehydration
■ Impaired leukocyte function leading to impaired wound healing and
increased risk of infection; greater antibiotic usage
Conditions that trigger hyperglycemia include:
■ Pancreatitis and other pancreatic and endocrine disorders
■ Sepsis
■ Pregnancy
■ Head injury
■ Glucocorticoid therapy
■ Immunosuppressants (e.g., tacrolimus, cyclosporine)
■ Sympathomimetic agents (e.g., norepinephrine, dopamine, dobutamine,
isoproterenol)
■ Enteral and parenteral nutrition
■ Liver or renal failure
■ Stress-induced insulin resistance or a hypermetabolic stress state; surgery
■ Dextrose containing IV infusions
Management
■ The American Diabetes Association (ADA) and the American Association of
Clinical Endocrinologists (AACE) now recommend the following serum glu-
cose targets for critically ill patients:
■ Serum glucose of 140–180 mg/dL is recommended.
■ Serum glucose of 110–140 mg/dL is acceptable in selected patients but
increases the risk of hypoglycemia.
■ For non–critically ill patients, the preprandial serum glucose target is
<140 mg/dL and the random serum glucose target is <180 mg/dL. In older
patients, the serum glucose target is 140–180 mg/dL. These may be consid-
ered target levels for transfer out of an ICU.
■ Insulin should not be started unless the patient exhibits persistent hyper-
glycemia (serum glucose >180 mg/dL).
■ Scheduled basal and meal insulin is recommended to improve glycemic
control compared with sliding-scale insulin coverage alone. Subcutaneous
insulin may be administered every 6 hr.
■ IV infusion of insulin is preferred to subcutaneous insulin administration.
216