Page 225 - Critical Care Notes
P. 225
4223_Tab08_216-229 29/08/14 8:26 AM Page 219
219
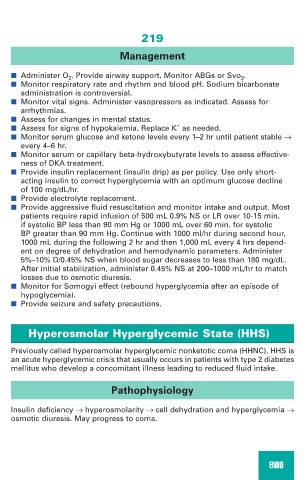
Management
■ Administer O 2 . Provide airway support. Monitor ABGs or Svo 2 .
■ Monitor respiratory rate and rhythm and blood pH. Sodium bicarbonate
administration is controversial.
■ Monitor vital signs. Administer vasopressors as indicated. Assess for
arrhythmias.
■ Assess for changes in mental status.
+
■ Assess for signs of hypokalemia. Replace K as needed.
■ Monitor serum glucose and ketone levels every 1–2 hr until patient stable →
every 4–6 hr.
■ Monitor serum or capillary beta-hydroxybutyrate levels to assess effective-
ness of DKA treatment.
■ Provide insulin replacement (insulin drip) as per policy. Use only short-
acting insulin to correct hyperglycemia with an optimum glucose decline
of 100 mg/dL/hr.
■ Provide electrolyte replacement.
■ Provide aggressive fluid resuscitation and monitor intake and output. Most
patients require rapid infusion of 500 mL 0.9% NS or LR over 10-15 min.
if systolic BP less than 90 mm Hg or 1000 mL over 60 min. for systolic
BP greater than 90 mm Hg. Continue with 1000 ml/hr during second hour,
1000 mL during the following 2 hr and then 1,000 mL every 4 hrs depend-
ent on degree of dehydration and hemodynamic parameters. Administer
5%–10% D/0.45% NS when blood sugar decreases to less than 180 mg/dL.
After initial stabilization, administer 0.45% NS at 200–1000 mL/hr to match
losses due to osmotic diuresis.
■ Monitor for Somogyi effect (rebound hyperglycemia after an episode of
hypoglycemia).
■ Provide seizure and safety precautions.
Hyperosmolar Hyperglycemic State (HHS)
Previously called hyperosmolar hyperglycemic nonketotic coma (HHNC), HHS is
an acute hyperglycemic crisis that usually occurs in patients with type 2 diabetes
mellitus who develop a concomitant illness leading to reduced fluid intake.
Pathophysiology
Insulin deficiency → hyperosmolarity → cell dehydration and hyperglycemia →
osmotic diuresis. May progress to coma.
ENDO