Page 44 - Critical Care Notes
P. 44
4223_Tab01_001-044 29/08/14 10:46 AM Page 38
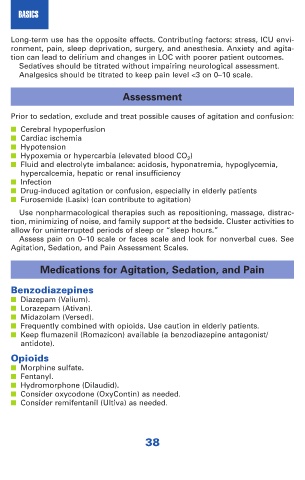
BASICS
Long-term use has the opposite effects. Contributing factors: stress, ICU envi-
ronment, pain, sleep deprivation, surgery, and anesthesia. Anxiety and agita-
tion can lead to delirium and changes in LOC with poorer patient outcomes.
Sedatives should be titrated without impairing neurological assessment.
Analgesics should be titrated to keep pain level <3 on 0–10 scale.
Assessment
Prior to sedation, exclude and treat possible causes of agitation and confusion:
■ Cerebral hypoperfusion
■ Cardiac ischemia
■ Hypotension
■ Hypoxemia or hypercarbia (elevated blood CO 2 )
■ Fluid and electrolyte imbalance: acidosis, hyponatremia, hypoglycemia,
hypercalcemia, hepatic or renal insufficiency
■ Infection
■ Drug-induced agitation or confusion, especially in elderly patients
■ Furosemide (Lasix) (can contribute to agitation)
Use nonpharmacological therapies such as repositioning, massage, distrac-
tion, minimizing of noise, and family support at the bedside. Cluster activities to
allow for uninterrupted periods of sleep or “sleep hours.”
Assess pain on 0–10 scale or faces scale and look for nonverbal cues. See
Agitation, Sedation, and Pain Assessment Scales.
Medications for Agitation, Sedation, and Pain
Benzodiazepines
■ Diazepam (Valium).
■ Lorazepam (Ativan).
■ Midazolam (Versed).
■ Frequently combined with opioids. Use caution in elderly patients.
■ Keep flumazenil (Romazicon) available (a benzodiazepine antagonist/
antidote).
Opioids
■ Morphine sulfate.
■ Fentanyl.
■ Hydromorphone (Dilaudid).
■ Consider oxycodone (OxyContin) as needed.
■ Consider remifentanil (Ultiva) as needed.
38