Page 58 - Critical Care Notes
P. 58
4223_Tab02_045-106 29/08/14 10:00 AM Page 52
CV
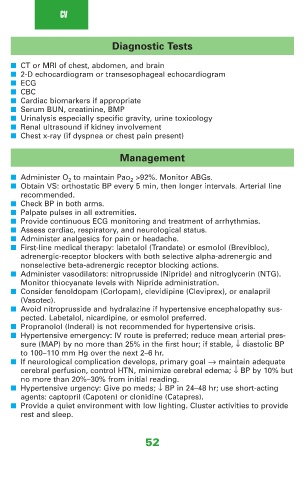
Diagnostic Tests
■ CT or MRI of chest, abdomen, and brain
■ 2-D echocardiogram or transesophageal echocardiogram
■ ECG
■ CBC
■ Cardiac biomarkers if appropriate
■ Serum BUN, creatinine, BMP
■ Urinalysis especially specific gravity, urine toxicology
■ Renal ultrasound if kidney involvement
■ Chest x-ray (if dyspnea or chest pain present)
Management
■ Administer O 2 to maintain PaO 2 >92%. Monitor ABGs.
■ Obtain VS: orthostatic BP every 5 min, then longer intervals. Arterial line
recommended.
■ Check BP in both arms.
■ Palpate pulses in all extremities.
■ Provide continuous ECG monitoring and treatment of arrhythmias.
■ Assess cardiac, respiratory, and neurological status.
■ Administer analgesics for pain or headache.
■ First-line medical therapy: labetalol (Trandate) or esmolol (Brevibloc),
adrenergic-receptor blockers with both selective alpha-adrenergic and
nonselective beta-adrenergic receptor blocking actions.
■ Administer vasodilators: nitroprusside (Nipride) and nitroglycerin (NTG).
Monitor thiocyanate levels with Nipride administration.
■ Consider fenoldopam (Corlopam), clevidipine (Cleviprex), or enalapril
(Vasotec).
■ Avoid nitroprusside and hydralazine if hypertensive encephalopathy sus-
pected. Labetalol, nicardipine, or esmolol preferred.
■ Propranolol (Inderal) is not recommended for hypertensive crisis.
■ Hypertensive emergency: IV route is preferred; reduce mean arterial pres-
sure (MAP) by no more than 25% in the first hour; if stable, ↓ diastolic BP
to 100–110 mm Hg over the next 2–6 hr.
■ If neurological complication develops, primary goal → maintain adequate
cerebral perfusion, control HTN, minimize cerebral edema; ↓ BP by 10% but
no more than 20%–30% from initial reading.
■ Hypertensive urgency: Give po meds; ↓ BP in 24–48 hr; use short-acting
agents: captopril (Capoten) or clonidine (Catapres).
■ Provide a quiet environment with low lighting. Cluster activities to provide
rest and sleep.
52