Page 89 - Critical Care Notes
P. 89
4223_Tab02_045-106 29/08/14 10:00 AM Page 83
83
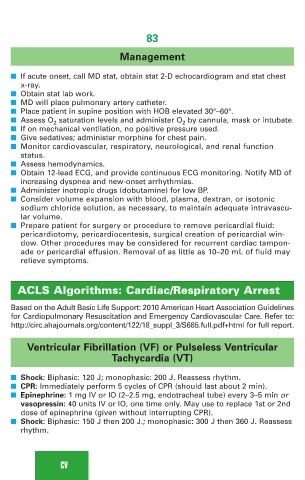
Management
■ If acute onset, call MD stat, obtain stat 2-D echocardiogram and stat chest
x-ray.
■ Obtain stat lab work.
■ MD will place pulmonary artery catheter.
■ Place patient in supine position with HOB elevated 30°–60°.
■ Assess O 2 saturation levels and administer O 2 by cannula, mask or intubate.
■ If on mechanical ventilation, no positive pressure used.
■ Give sedatives; administer morphine for chest pain.
■ Monitor cardiovascular, respiratory, neurological, and renal function
status.
■ Assess hemodynamics.
■ Obtain 12-lead ECG, and provide continuous ECG monitoring. Notify MD of
increasing dyspnea and new-onset arrhythmias.
■ Administer inotropic drugs (dobutamine) for low BP.
■ Consider volume expansion with blood, plasma, dextran, or isotonic
sodium chloride solution, as necessary, to maintain adequate intravascu-
lar volume.
■ Prepare patient for surgery or procedure to remove pericardial fluid:
pericardiotomy, pericardiocentesis, surgical creation of pericardial win-
dow. Other procedures may be considered for recurrent cardiac tampon-
ade or pericardial effusion. Removal of as little as 10–20 mL of fluid may
relieve symptoms.
ACLS Algorithms: Cardiac/Respiratory Arrest
Based on the Adult Basic Life Support: 2010 American Heart Association Guidelines
for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Refer to:
http://circ.ahajournals.org/content/122/18_suppl_3/S685.full.pdf+html for full report.
Ventricular Fibrillation (VF) or Pulseless Ventricular
Tachycardia (VT)
■ Shock: Biphasic: 120 J; monophasic: 200 J. Reassess rhythm.
■ CPR: Immediately perform 5 cycles of CPR (should last about 2 min).
■ Epinephrine: 1 mg IV or IO (2–2.5 mg, endotracheal tube) every 3–5 min or
vasopressin: 40 units IV or IO, one time only. May use to replace 1st or 2nd
dose of epinephrine (given without interrupting CPR).
■ Shock: Biphasic: 150 J then 200 J.; monophasic: 300 J then 360 J. Reassess
rhythm.
CV