Page 108 - ACCCN's Critical Care Nursing
P. 108
Ethical Issues in Critical Care 85
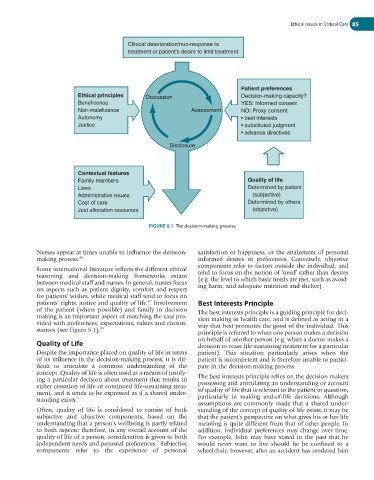
Clinical deterioration/non-response to
treatment or patient’s desire to limit treatment
Patient preferences
Ethical principles Discussion Decision-making capacity?
Beneficence YES: Informed consent
Non-maleficence Assessment NO: Proxy consent
Autonomy • best interests
Justice • substituted judgment
• advance directives
Disclosure
Contextual features
Family members Quality of life
Laws Determined by patient
Administrative issues (subjective)
Cost of care Determined by others
Just allocation resources (objective)
FIGURE 5.1 The decision-making process.
Nurses appear at times unable to influence the decision- satisfaction or happiness, or the attainment of personal
making process. 46 informed desires or preferences. Conversely, objective
components refer to factors outside the individual, and
Some international literature reflects the different ethical
reasoning and decision-making frameworks extant tend to focus on the notion of ‘need’ rather than desires
between medical staff and nurses. In general, nurses focus (e.g. the level to which basic needs are met, such as avoid-
on aspects such as patient dignity, comfort and respect ing harm, and adequate nutrition and shelter).
for patients’ wishes, while medical staff tend to focus on
patients’ rights, justice and quality of life. Involvement Best Interests Principle
47
of the patient (where possible) and family in decision The best interests principle is a guiding principle for deci-
making is an important aspect of matching the care pro- sion making in health care, and is defined as acting in a
vided with preferences, expectations, values and circum- way that best promotes the good of the individual. This
stances (see Figure 5.1). 48
principle is referred to when one person makes a decision
Quality of Life on behalf of another person (e.g. when a doctor makes a
decision to cease life-sustaining treatment for a particular
Despite the importance placed on quality of life in terms patient). This situation particularly arises when the
of its influence in the decision-making process, it is dif- patient is incompetent and is therefore unable to partici-
ficult to articulate a common understanding of the pate in the decision-making process.
concept. Quality of life is often used as a means of justify-
ing a particular decision about treatment that results in The best interests principle relies on the decision makers
either cessation of life or continued life-sustaining treat- possessing and articulating an understanding or account
ment, and it tends to be expressed as if a shared under- of quality of life that is relevant to the patient in question,
standing exists. 4 particularly in making end-of-life decisions. Although
assumptions are commonly made that a shared under-
Often, quality of life is considered to consist of both standing of the concept of quality of life exists, it may be
subjective and objective components, based on the that the patient’s perspective on what gives his or her life
understanding that a person’s wellbeing is partly related meaning is quite different from that of other people. In
to both aspects; therefore, in any overall account of the addition, individual preferences may change over time.
quality of life of a person, consideration is given to both For example, John may have stated in the past that he
9
independent needs and personal preferences. Subjective would never want to live should he be confined to a
components refer to the experience of personal wheelchair; however, after an accident has rendered him