Page 2181 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 2181
1934 Part XII Hemostasis and Thrombosis
ADP
Thrombin Outside-In signaling
Epinephrine by integrins Receptors
PAF coupled to
Thromboxane A2 tyrosine
ADP Receptors coupled to G-protein kinases
2+
Receptors coupled to induced Ca increase via PLC VCL
G protein–induced inhibition activation (e.g., P2Y1) ATA
of adenyl cyclase (e.g., P2Y 12) Ridogrel GPIb-IX-V Shear
Ticlopidine Complex stress
Clopidogrel (via) vWF
Receptors coupled to
G protein–induced stimulation γ PIP2
of adenyl cyclase γ α β
β Src
Adenyl α PLCβ2 PLCγ PI3
Epoprostenol cyclase FAK kinase Collagen
IIioprost ATP GPVI
Beraprost IP3 DAG Focal contact ITAM
γ formation ITAM
β ITAM Immune
α IP3 Syk FcRγ-chains ITAM complexes
FcγRII
2+
Ca
Guanyl cyclase
cGMP
LAT,ZAP,70,Vav SLP-76,
NO, cAMP sequestration Ca 2+ Ca 2+ Ca 2+ and other phosphotyrosine Syk FcRγ-chains
Nitrates Dense tubular system kinases and adaptors
Nitroprusside GTP Ca 2+ Ca 2+ PI3K
Dense
granule Pleckstrin Protein kinase C
Release reaction phosphorylation MLCK
ADP ADP Cytosolic Ca 2+ Myosin
5-HT 5-HT phosphorylation
Phospholipase A2 Activation of phosholipase A2
Arachidonic acid GP IIb/IIIa activation
Cyclooxygenase Aspirin Platelet
Cyclic endoperoxide aggregation
2+
Thromboxane synthase Ridogrel Ca -Induced
conformational
Thromboxane A 2 changes
Scramblase activation Abciximab
(transbilayer movement of Eptifibatide
procoagulant phospholipid) Tirofiban
GP IIb/IIIa complex
Thromboxane A 2
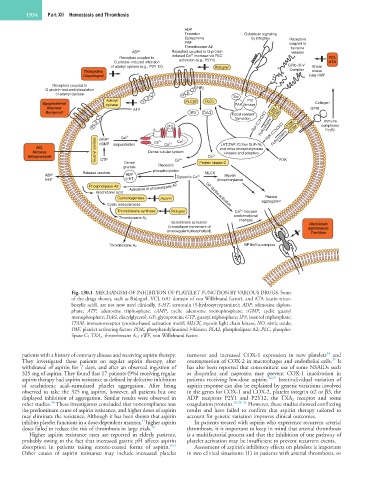
Fig. 130.1 MECHANISM OF INHIBITION OF PLATELET FUNCTION BY VARIOUS DRUGS. Some
of the drugs shown, such as Ridogrel, VCL (rA1 domain of von Willebrand factor), and ATA (aurin tricar-
boxylic acid), are not now used clinically. 5-HT, serotonin (5-hydroxytryptamine); ADP, adenosine diphos-
phate; ATP, adenosine triphosphate; cAMP, cyclic adenosine monophosphate; cGMP, cyclic guanyl
monophosphate; DAG, diacylglycerol; GP, glycoprotein; GTP, guanyl triphosphate; IP3, inositol triphosphate;
ITAM, immunoreceptor tyrosine-based activation motif; MLCK, myosin light chain kinase; NO, nitric oxide;
PAF, platelet activating factor; PI3K, phosphatidylinositol 3-kinase; PLA2, phospholipase A2; PLC, phospho-
lipase C; TXA 2 , thromboxane A 2 ; vWF, von Willebrand factor.
34
patients with a history of coronary disease and receiving aspirin therapy. turnover and increased COX-1 expression in new platelets and
35
They investigated these patients on regular aspirin therapy, after overexpression of COX-2 in macrophages and endothelial cells. It
withdrawal of aspirin for 7 days, and after an observed ingestion of has also been reported that concomitant use of some NSAIDs such
325 mg of aspirin. They found that 17 patients (9%) receiving regular as ibuprofen and naproxen may prevent COX-1 inactivation in
aspirin therapy had aspirin resistance as defined by defective inhibition patients receiving low-dose aspirin. 36,37 Interindividual variation of
of arachidonic acid–stimulated platelet aggregation. After being aspirin response can also be explained by genetic variations involved
observed to take the 325 mg aspirin, however, all patients but one in the genes for COX-1 and COX-2, platelet integrin α2 or β3, the
displayed inhibition of aggregation. Similar results were observed in ADP receptors P2Y1 and P2Y12, the TXA 2 receptor and some
30
other studies. These investigators concluded that noncompliance was coagulation proteins. 26,38–41 However, these studies showed conflicting
the predominant cause of aspirin resistance, and higher doses of aspirin results and have failed to confirm that aspirin therapy tailored to
may eliminate the resistance. Although it has been shown that aspirin account for genetic variation improves clinical outcomes.
31
inhibits platelet functions in a dose-dependent manner, higher aspirin In patients treated with aspirin who experience recurrent arterial
doses failed to reduce the risk of thrombosis in large trials. 32 thrombosis, it is important to keep in mind that arterial thrombosis
Higher aspirin resistance rates are reported in elderly patients, is a multifactorial process and that the inhibition of one pathway of
probably owing to the fact that increased gastric pH affects aspirin platelet activation may be insufficient to prevent recurrent events.
absorption in patients taking enteric-coated forms of aspirin. 8,33 Assessment of aspirin’s inhibitory effects on platelets is important
Other causes of aspirin resistance may include increased platelet in two clinical situations: (1) in patients with arterial thrombosis, or