Page 236 - Critical Care Notes
P. 236
4223_Tab09_230-248 29/08/14 8:26 AM Page 230
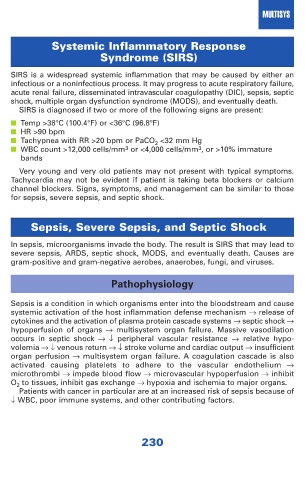
MULTISYS
Systemic Inflammatory Response
Syndrome (SIRS)
SIRS is a widespread systemic inflammation that may be caused by either an
infectious or a noninfectious process. It may progress to acute respiratory failure,
acute renal failure, disseminated intravascular coagulopathy (DIC), sepsis, septic
shock, multiple organ dysfunction syndrome (MODS), and eventually death.
SIRS is diagnosed if two or more of the following signs are present:
■ Temp >38°C (100.4°F) or <36°C (96.8°F)
■ HR >90 bpm
■ Tachypnea with RR >20 bpm or PaCO 2 <32 mm Hg
■ WBC count >12,000 cells/mm 3 or <4,000 cells/mm 3 , or >10% immature
bands
Very young and very old patients may not present with typical symptoms.
Tachycardia may not be evident if patient is taking beta blockers or calcium
channel blockers. Signs, symptoms, and management can be similar to those
for sepsis, severe sepsis, and septic shock.
Sepsis, Severe Sepsis, and Septic Shock
In sepsis, microorganisms invade the body. The result is SIRS that may lead to
severe sepsis, ARDS, septic shock, MODS, and eventually death. Causes are
gram-positive and gram-negative aerobes, anaerobes, fungi, and viruses.
Pathophysiology
Sepsis is a condition in which organisms enter into the bloodstream and cause
systemic activation of the host inflammation defense mechanism → release of
cytokines and the activation of plasma protein cascade systems → septic shock →
hypoperfusion of organs → multisystem organ failure. Massive vasodilation
occurs in septic shock → ↓ peripheral vascular resistance → relative hypo -
volemia →↓ venous return →↓ stroke volume and cardiac output → insufficient
organ perfusion → multisystem organ failure. A coagulation cascade is also
activated causing platelets to adhere to the vascular endothelium →
microthrombi → impede blood flow → microvascular hypoperfusion → inhibit
O 2 to tissues, inhibit gas exchange → hypoxia and ischemia to major organs.
Patients with cancer in particular are at an increased risk of sepsis because of
↓ WBC, poor immune systems, and other contributing factors.
230