Page 415 - Cardiac Nursing
P. 415
/09
/09
/09
1
1:2
1
1
A
6
6
xd
/29
p
p
/29
1:2
e 3
g
g
e 3
A
91
91
g
M
4 P
4 P
M
Pa
Pa
Pa
xd
a
a
a
a
ara
t
p
ara
t
In
LWB
K34
LWB K34 0-c 17_ pp388-399.qxd 6/29/09 11:24 PM Page 391 Aptara Inc.
LWBK340-c17_
0-c
c.
In
17_
c.
q
q
q
99.
99.
8-3
38
p
38
8-3
p
C HAPTER 1 7 / Heart Rate Variability 391
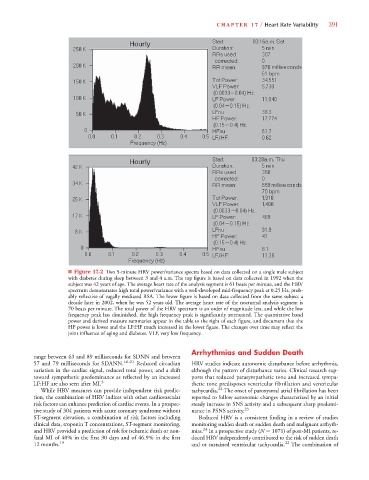
■ Figure 17-2 Two 5-minute HRV power/variance spectra based on data collected on a single male subject
with diabetes during sleep between 3 and 4 a.m. The top figure is based on data collected in 1992 when the
subject was 42 years of age. The average heart rate of the analysis segment is 61 beats per minute, and the HRV
spectrum demonstrates high total power/variance with a well-developed mid-frequency peak at 0.25 Hz, prob-
ably reflective of vagally mediated RSA. The lower figure is based on data collected from the same subject a
decade later in 2002, when he was 52 years old. The average heart rate of the nocturnal analysis segment is
70 beats per minute. The total power of the HRV spectrum is an order of magnitude less, and while the low
frequency peak has diminished, the high frequency peak is significantly attenuated. The quantitative band
power and derived measure summaries appear in the table to the right of each figure, and document that the
HF power is lower and the LF:HF much increased in the lower figure. The changes over time may reflect the
joint influence of aging and diabetes. VLF, very low frequency.
Arrhythmias and Sudden Death
range between 63 and 89 milliseconds for SDNN and between
57 and 79 milliseconds for SDANN. 16,21 Reduced circadian HRV studies indicate autonomic disturbance before arrhythmia,
variation in the cardiac signal, reduced total power, and a shift although the pattern of disturbance varies. Clinical research sup-
toward sympathetic predominance as reflected by an increased ports that reduced parasympathetic tone and increased sympa-
LF:HF are also seen after MI. 3 thetic tone predisposes ventricular fibrillation and ventricular
22
While HRV measures can provide independent risk predic- tachycardia. The onset of paroxysmal atrial fibrillation has been
tion, the combination of HRV indices with other cardiovascular reported to follow autonomic changes characterized by an initial
risk factors can enhance prediction of cardiac events. In a prospec- steady increase in SNS activity and a subsequent sharp predomi-
tive study of 304 patients with acute coronary syndrome without nance in PSNS activity. 23
ST-segment elevation, a combination of risk factors including Reduced HRV is a consistent finding in a review of studies
clinical data, troponin T concentrations, ST-segment monitoring, monitoring sudden death or sudden death and malignant arrhyth-
24
and HRV provided a prediction of risk for ischemic death or non- mias. In a prospective study (N 1071) of post-MI patients, re-
fatal MI of 40% in the first 30 days and of 46.9% in the first duced HRV independently contributed to the risk of sudden death
12 months. 19 and or sustained ventricular tachycardia. 22 The combination of