Page 436 - Cardiac Nursing
P. 436
pta
M
41
2 A
P
6
qxd
P
/09
p40
ra
19.
0-4
Inc
a
a
/30
:57
K34
0-c
18_
LWB K34 0-c 18_ p40 0-4 19. qxd 6 /30 /09 7 7 :57 P M P a g g e e 41 2 A pta ra Inc . .
LWBK340-c18_p400-419.qxd 6/30/09 7:57 PM Page 412 Aptara Inc.
LWB
412 P A R T III / Assessment of Heart Disease
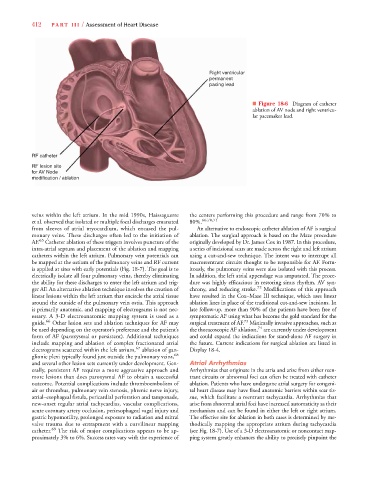
Right ventricular
permanent
pacing lead
■ Figure 18-6 Diagram of catheter
ablation of AV node and right ventricu-
lar pacemaker lead.
R RF catheter
R RF lesion site
o
for AV Node
m modification / ablation
veins within the left atrium. In the mid 1990s, Haissaguerre the centers performing this procedure and range from 70% to
et al. observed that isolated or multiple focal discharges emanated 80%. 66,70,71
from sleeves of atrial myocardium, which encased the pul- An alternative to endoscopic catheter ablation of AF is surgical
monary veins. These discharges often led to the initiation of ablation. The surgical approach is based on the Maze procedure
AF. 65 Catheter ablation of these triggers involves puncture of the originally developed by Dr. James Cox in 1987. In this procedure,
intra-atrial septum and placement of the ablation and mapping a series of incisional scars are made across the right and left atrium
catheters within the left atrium. Pulmonary vein potentials can using a cut-and-sew technique. The intent was to interrupt all
be mapped at the ostium of the pulmonary veins and RF current macroreentrant circuits thought to be responsible for AF. Fortu-
is applied at sites with early potentials (Fig. 18-7). The goal is to itously, the pulmonary veins were also isolated with this process.
electrically isolate all four pulmonary veins, thereby eliminating In addition, the left atrial appendage was amputated. The proce-
the ability for these discharges to enter the left atrium and trig- dure was highly efficacious in restoring sinus rhythm, AV syn-
ger AF. An alternative ablation technique involves the creation of chrony, and reducing stroke. 72 Modifications of this approach
linear lesions within the left atrium that encircle the atrial tissue have resulted in the Cox–Maze III technique, which uses linear
around the outside of the pulmonary vein ostia. This approach ablation lines in place of the traditional cut-and-sew incisions. In
is primarily anatomic, and mapping of electrograms is not nec- late follow-up, more than 90% of the patients have been free of
essary. A 3-D electroanatomic mapping system is used as a symptomatic AF using what has become the gold standard for the
73
guide. 66 Other lesion sets and ablation techniques for AF may surgical treatment of AF. Minimally invasive approaches, such as
74
be used depending on the operator’s preference and the patient’s the thoracoscopic AF ablation, are currently under development
form of AF (paroxysmal or persistent). Additional techniques and could expand the indications for stand-alone AF surgery in
include mapping and ablation of complex fractionated atrial the future. Current indications for surgical ablation are listed in
electrograms scattered within the left atrium, 67 ablation of gan- Display 18-4.
glionic plexi typically found just outside the pulmonary veins, 68
and several other lesion sets currently under development. Gen- Atrial Arrhythmias
erally, persistent AF requires a more aggressive approach and Arrhythmias that originate in the atria and arise from either reen-
more lesions than does paroxysmal AF to obtain a successful trant circuits or abnormal foci can often be treated with catheter
outcome. Potential complications include thromboembolism of ablation. Patients who have undergone atrial surgery for congeni-
air or thrombus, pulmonary vein stenosis, phrenic nerve injury, tal heart disease may have fixed anatomic barriers within scar tis-
atrial–esophageal fistula, pericardial perforation and tamponade, sue, which facilitate a reentrant tachycardia. Arrhythmias that
new-onset regular atrial tachycardias, vascular complications, arise from abnormal atrial foci have increased automaticity as their
acute coronary artery occlusion, periesophageal vagal injury and mechanism and can be found in either the left or right atrium.
gastric hypomotility, prolonged exposure to radiation and mitral The effective site for ablation in both cases is determined by me-
valve trauma due to entrapment with a curvilinear mapping thodically mapping the appropriate atrium during tachycardia
catheter. 69 The risk of major complications appears to be ap- (see Fig. 18-7). Use of a 3-D electroanatomic or noncontact map-
proximately 3% to 6%. Success rates vary with the experience of ping system greatly enhances the ability to precisely pinpoint the