Page 1642 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 1642
Chapter 90 Psychosocial Aspects of Hematologic Disorders 1463
Initial symptoms Factors That May Predict Poor Coping in Patients With
BOX 90.1 Cancer
Past psychiatric history
Workup Diagnosis
Compliance issues
Demographic factors such as younger age and female sex
Limited social support or difficult social relationships
Recent history of smoking cessation
No curative attempt Curative attempt Substance abuse history
Recent losses
Advanced disease
Progressive disease Remission No response Uncontrolled symptoms
Pessimistic outlook on life
Multiple obligations
Avoidance coping (escape-avoidance, distancing, and denial)
Death Lower functional status
Relapse
Higher regimen-related toxicity
Treatment
diagnosis of cancer are vital. Patients who have a pervasive and
unyielding negative affect that persists long after the crisis of diagnosis
Remission may require ongoing psychosocial monitoring and referral for services
and supportive interventions throughout their treatment and disease
Long-term Progressive 24
survival disease course.
In addition, family assessment during this phase is vital. Levels of
family distress, depression, and anxiety are mediated by the function-
24
Death ing of the family at the time of diagnosis. Studies have shown that
24
caregivers and families share similar rates of psychosocial angst.
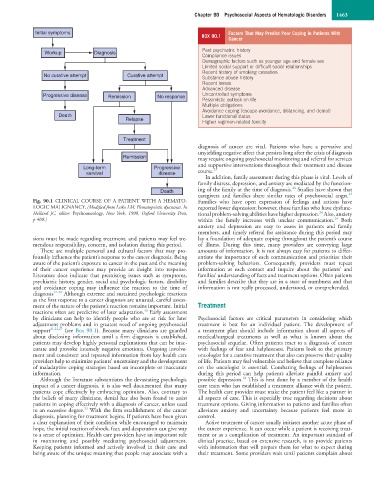
Fig. 90.1 CLINICAL COURSE OF A PATIENT WITH A HEMATO- Families who have open expression of feelings and actions have
LOGIC MALIGNANCY. (Modified from Lesko LM: Hematopoietic dyscrasias. In reported lower depression; however, those families who have dysfunc-
Holland JC, editor: Psychooncology, New York, 1998, Oxford University Press, tional problem-solving abilities have higher depression. Also, anxiety
24
24
p 408.) within the family increases with unclear communication. Both
anxiety and depression are easy to assess in patients and family
members, and timely referral for assistance during this period may
sions must be made regarding treatment, and patients may feel tre- lay a foundation of adequate coping throughout the patient’s course
mendous responsibility, concern, and isolation during this period. of illness. During this time, many providers are conveying large
There are multiple personal and cultural factors that may pro- amounts of information. It is not always easy for patients to differ-
foundly influence the patient’s response to the cancer diagnosis. Being entiate the importance of each communication and prioritize their
aware of the patient’s exposure to cancer in the past and the meaning problem-solving behaviors. Consequently, providers must repeat
of their cancer experience may provide an insight into response. information at each contact and inquire about the patients’ and
Literature does indicate that preexisting issues such as symptoms, families’ understanding of facts and treatment options. Often patients
psychiatric history, gender, social and psychologic factors, disability and families describe that they are in a state of numbness and that
and avoidance coping may influence the reaction to the time of information is not really processed, understood, or comprehended.
diagnosis 17–20 Although extreme and sustained psychologic reactions
as the first response to a cancer diagnosis are unusual, careful assess-
ment of the nature of the patient’s reaction remains important. Initial Treatment
43
reactions often are predictive of later adaptation. Early assessment
by clinicians can help to identify people who are at risk for later Psychosocial factors are critical parameters in considering which
adjustment problems and in greatest need of ongoing psychosocial treatment is best for an individual patient. The development of
support 21,22,27 (see Box 90.1). Because many clinicians are guarded a treatment plan should include information about all aspects of
about disclosing information until a firm diagnosis is established, medical/surgical treatments as well as what is known about the
patients may develop highly personal explanations that can be inac- psychosocial sequelae. Often patients react to a diagnosis of cancer
curate and provoke intensely negative emotions. Ongoing involve- with feelings of fear and helplessness. Patients look to the primary
ment and consistent and repeated information from key health care oncologist for a curative treatment that also can preserve their quality
providers help to minimize patients’ uncertainty and the development of life. Patients may feel vulnerable and believe that complete reliance
of maladaptive coping strategies based on incomplete or inaccurate on the oncologist is essential. Combating feelings of helplessness
information. during this period can help patients alleviate painful anxiety and
18
Although the literature substantiates the devastating psychologic possible depression. This is best done by a member of the health
impact of a cancer diagnosis, it is also well documented that many care team who has established a treatment alliance with the patient.
patients cope effectively by embracing optimism. Also, contrary to The health care provider must make the patient feel like a partner in
the beliefs of many clinicians, denial has also been found to assist all aspects of care. This is especially true regarding decisions about
patients in coping effectively with a diagnosis of cancer, unless used treatment options. Giving information to patients and families often
23
to an excessive degree. With the firm establishment of the cancer alleviates anxiety and uncertainty because patients feel more in
diagnosis, planning for treatment begins. If patients have been given control.
a clear explanation of their condition while encouraged to maintain Active treatment of cancer usually initiates another acute phase of
hope, the initial reaction of shock, fear, and desperation can give way the cancer experience. It can occur while a patient is receiving treat-
to a sense of optimism. Health care providers have an important role ment or as a complication of treatment. An important standard of
in monitoring and possibly mediating psychosocial adjustment. clinical practice, based on extensive research, is to provide patients
Keeping patients informed and actively involved in their care and with information that will prepare them for what to expect during
being aware of the unique meaning that people may associate with a their treatment. Some providers wait until patients complain about