Page 2154 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 2154
Chapter 127 Regulatory Mechanisms in Hemostasis 1907
Platelets Activated
(PARs) Platelets
Fibrinogen
Prothrombin fIIa
fXIII Fibrin
fXIIIa
Crosslinked
TFPI fXa + fVa fV Fibrin polymer
fXI
APC AT
fIXa + fVIIIa fVIII
fX
TF+fVIIa fXIa
fIX
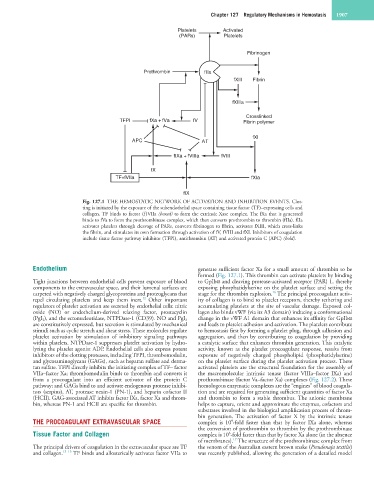
Fig. 127.1 THE HEMOSTATIC NETWORK OF ACTIVATION AND INHIBITION EVENTS. Clot-
ting is initiated by the exposure of the subendothelial space containing tissue factor (TF)–expressing cells and
collagen. TF binds to factor (f)VIIa (boxed) to form the extrinsic Xase complex. The fXa that is generated
binds to fVa to form the prothrombinase complex, which then converts prothrombin to thrombin (fIIa). fIIa
activates platelets through cleavage of PARs, converts fibrinogen to fibrin, activates fXIII, which cross-links
the fibrin, and stimulates its own formation through activation of fV, fVIII and fXI. Inhibitors of coagulation
include tissue factor pathway inhibitor (TFPI), antithrombin (AT) and activated protein C (APC) (bold).
Endothelium generate sufficient factor Xa for a small amount of thrombin to be
formed (Fig. 127.1). This thrombin can activate platelets by binding
Tight junctions between endothelial cells prevent exposure of blood to GpIbα and cleaving protease-activated receptor (PAR) 1, thereby
components to the extravascular space, and their lumenal surfaces are exposing phosphatidylserine on the platelet surface and setting the
16
carpeted with negatively charged glycoproteins and proteoglycans that stage for the thrombin explosion. The principal procoagulant activ-
12
repel circulating platelets and keep them inert. Other important ity of collagen is to bind to platelet receptors, thereby tethering and
regulators of platelet activation are secreted by endothelial cells: nitric accumulating platelets at the site of vascular damage. Exposed col-
oxide (NO) or endothelium-derived relaxing factor, prostacyclin lagen also binds vWF (via its A3 domain) inducing a conformational
(PgI 2 ), and the ectonucleotidase, NTPDase-1 (CD39). NO and PgI 2 change in the vWF A1 domain that enhances its affinity for GpIbα
are constitutively expressed, but secretion is stimulated by mechanical and leads to platelet adhesion and activation. The platelets contribute
stimuli such as cyclic stretch and shear stress. These molecules regulate to hemostasis first by forming a platelet plug, through adhesion and
platelet activation by stimulation of inhibitory signaling pathways aggregation, and then by contributing to coagulation by providing
within platelets. NTPDase-1 suppresses platelet activation by hydro- a catalytic surface that enhances thrombin generation. This catalytic
lyzing the platelet agonist ADP. Endothelial cells also express potent activity, known as the platelet procoagulant response, results from
inhibitors of the clotting proteases, including TFPI, thrombomodulin, exposure of negatively charged phospholipid (phosphatidylserine)
and glycosaminoglycans (GAGs), such as heparan sulfate and derma- on the platelet surface during the platelet activation process. These
tan sulfate. TFPI directly inhibits the initiating complex of TF– factor activated platelets are the structural foundation for the assembly of
VIIa–factor Xa; thrombomodulin binds to thrombin and converts it the macromolecular intrinsic tenase (factor VIIIa–factor IXa) and
from a procoagulant into an efficient activator of the protein C prothrombinase (factor Va–factor Xa) complexes (Fig. 127.2). These
pathway; and GAGs bind to and activate endogenous protease inhibi- homologous enzymatic complexes are the “engines” of blood coagula-
tors (serpins), AT, protease nexin-1 (PN-1), and heparin cofactor II tion and are required for generating sufficient quantities of factor Xa
(HCII). GAG-associated AT inhibits factor IXa, factor Xa and throm- and thrombin to form a stable thrombus. The anionic membrane
bin, whereas PN-1 and HCII are specific for thrombin. helps to capture, orient and approximate the enzymes, cofactors and
substrates involved in the biological amplification process of throm-
bin generation. The activation of factor X by the intrinsic tenase
THE PROCOAGULANT EXTRAVASCULAR SPACE complex is 10 -fold faster than that by factor IXa alone, whereas
9
the conversion of prothrombin to thrombin by the prothrombinase
Tissue Factor and Collagen complex is 10 -fold faster than that by factor Xa alone (in the absence
6
17
of membranes). The structure of the prothrombinase complex from
The principal drivers of coagulation in the extravascular space are TF the venom of the Australian eastern brown snake (Pseudonaja textilis)
and collagen. 13–15 TF binds and allosterically activates factor VIIa to was recently published, allowing the generation of a detailed model