Page 2364 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 2364
2106 Part XII Hemostasis and Thrombosis
nonspecific abnormalities may be detected. Patients with pulmonary
Clinically suspected DVT
infarction or atelectasis may have reduced movement of the affected
portion of the chest.
CUS
Differential Diagnosis
- + Treat The differential diagnosis of dyspnea and pleuritic chest pain, in
addition to PE, includes pneumonia, pleurisy, chest wall pain, peri-
carditis, atelectasis, pneumothorax, acute bronchitis, acute bronchi-
Serial CUS olitis, and acute bronchial obstruction as a result of mucous plugging
or bronchoconstriction.
A Exclude Dx - +
Diagnosis
Clinically suspected DVT The clinical diagnosis of PE requires objective testing. The chest
radiograph is not specific for PE and usually does not show any
diagnostic abnormality. Nevertheless, it is useful in excluding other
causes for the presenting symptoms (e.g., pneumothorax) and is
Pretest probability essential for interpreting V/Q lung scan findings. The electrocardio-
gram (ECG) is frequently normal or may show nonspecific abnor-
malities (e.g., sinus tachycardia). However, in the appropriate clinical
Low Moderate or high setting, ECG evidence of right ventricular strain is strongly suggestive
of PE. Elevated levels of cardiac troponin, brain natriuretic peptide
(BNP) or N-terminal pro-BNP (NT-proBNP) can result from right
Validated D-dimer CUS ventricular strain and associated cardiomyocyte stretch.
- Diagnosis - + OBJECTIVE DIAGNOSTIC TESTS FOR
excluded Treat
PULMONARY EMBOLISM
+ - Serial Pulmonary Angiography
CUS
B CUS Although pulmonary angiography is the reference standard for
establishing the presence or absence of PE, it is no longer routinely
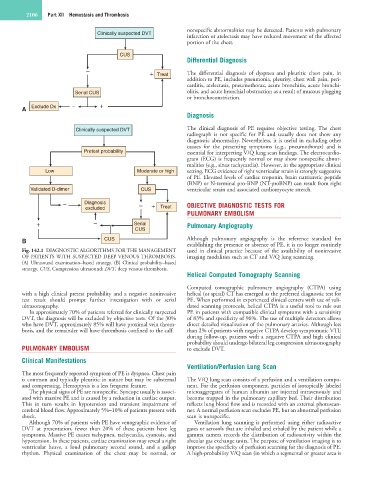
Fig. 142.1 DIAGNOSTIC ALGORITHMS FOR THE MANAGEMENT used in clinical practice because of the availability of noninvasive
OF PATIENTS WITH SUSPECTED DEEP VENOUS THROMBOSIS. imaging modalities such as CT and V/Q lung scanning.
(A) Ultrasound examination–based strategy. (B) Clinical probability–based
strategy. CUS, Compression ultrasound; DVT, deep venous thrombosis.
Helical Computed Tomography Scanning
Computed tomographic pulmonary angiography (CTPA) using
with a high clinical pretest probability and a negative noninvasive helical (or spiral) CT has emerged as the preferred diagnostic test for
test result should prompt further investigation with or serial PE. When performed in experienced clinical centers with use of vali-
ultrasonography. dated scanning protocols, helical CTPA is a useful tool to rule out
In approximately 70% of patients referred for clinically suspected PE in patients with compatible clinical symptoms with a sensitivity
DVT, the diagnosis will be excluded by objective tests. Of the 30% of 83% and specificity of 96%. The use of multiple detectors allows
who have DVT, approximately 85% will have proximal vein throm- direct detailed visualization of the pulmonary arteries. Although less
bosis, and the remainder will have thrombosis confined to the calf. than 2% of patients with negative CTPA develop symptomatic VTE
during follow-up, patients with a negative CTPA and high clinical
probability should undergo bilateral leg compression ultrasonography
PULMONARY EMBOLISM to exclude DVT.
Clinical Manifestations
Ventilation/Perfusion Lung Scan
The most frequently reported symptom of PE is dyspnea. Chest pain
is common and typically pleuritic in nature but may be substernal The V/Q lung scan consists of a perfusion and a ventilation compo-
and compressing. Hemoptysis is a less frequent feature. nent. For the perfusion component, particles of isotopically labeled
The physical signs of PE are nonspecific. Syncope usually is associ- microaggregates of human albumin are injected intravenously and
ated with massive PE and is caused by a reduction in cardiac output. become trapped in the pulmonary capillary bed. Their distribution
This in turn results in hypotension and transient impairment of reflects lung blood flow and is recorded with an external photoscan-
cerebral blood flow. Approximately 5%–10% of patients present with ner. A normal perfusion scan excludes PE, but an abnormal perfusion
shock. scan is nonspecific.
Although 70% of patients with PE have venographic evidence of Ventilation lung scanning is performed using either radioactive
DVT at presentation, fewer than 20% of these patients have leg gases or aerosols that are inhaled and exhaled by the patient while a
symptoms. Massive PE causes tachypnea, tachycardia, cyanosis, and gamma camera records the distribution of radioactivity within the
hypotension. In these patients, cardiac examination may reveal a right alveolar gas exchange units. The purpose of ventilation imaging is to
ventricular heave, a loud pulmonary second sound, and a gallop improve the specificity of perfusion scanning for the diagnosis of PE.
rhythm. Physical examination of the chest may be normal, or A high-probability V/Q scan (in which a segmental or greater area is