Page 577 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 577
492 Part V Red Blood Cells
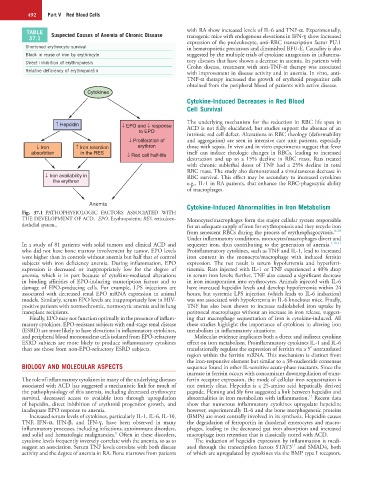
TABLE Suspected Causes of Anemia of Chronic Disease with RA show increased levels of IL-6 and TNF-α. Experimentally,
37.1 transgenic mice with endogenous elevations in IFN-ɣ show increased
expression of the proleukocyte, anti-RBC transcription factor PU.1
Shortened erythrocyte survival in hematopoietic precursors and diminished BFU-E. Causality is also
Block in reuse of iron by erythrocyte suggested by the multiple trials of cytokine antagonists in inflamma-
Direct inhibition of erythropoiesis tory diseases that have shown a decrease in anemia. In patients with
Crohn disease, treatment with anti-TNF-α therapy was associated
Relative deficiency of erythropoietin with improvement in disease activity and in anemia. In vitro, anti-
TNF-α therapy increased the growth of erythroid progenitor cells
obtained from the peripheral blood of patients with active disease.
Cytokines
Cytokine-Induced Decreases in Red Blood
Cell Survival
↑ Hepcidin ↓ EPO and ↓ response The underlying mechanism for the reduction in RBC life span in
to EPO ACD is not fully elucidated, but studies support the absence of an
intrinsic red cell defect. Alterations in RBC rheology (deformability
↓ Proliferation of and aggregation) are seen in intensive care unit patients, especially
↓ Iron ↑ Iron retention erythron those with sepsis. In vivo and in vitro experiments suggest that fever
absorbtion in the RES ↓ Red cell half-life itself can induce rheologic changes in RBCs, leading to increased
destruction and up to a 15% decline in RBC mass. Rats treated
with chronic sublethal doses of TNF had a 25% decline in total
RBC mass. The study also demonstrated a simultaneous decrease in
↓ Iron availability in RBC survival. This effect may be secondary to increased cytokines
the erythron e.g., IL-1 in RA patients, that enhance the RBC-phagocytic ability
of macrophages.
Anemia Cytokine-Induced Abnormalities in Iron Metabolism
Fig. 37.1 PATHOPHYSIOLOGIC FACTORS ASSOCIATED WITH
THE DEVELOPMENT OF ACD. EPO, Erythropoietin; RES, reticuloen- Monocytes/macrophages form the major cellular system responsible
dothelial system,. for an adequate supply of iron for erythropoiesis and they recycle iron
from senescent RBCs during the process of erythrophagocytosis. 8–10
Under inflammatory conditions, monocytes/macrophages divert and
In a study of 81 patients with solid tumors and clinical ACD and sequester iron, thus contributing to the generation of anemia. 1,10,11
who did not have bone marrow involvement by tumor, EPO levels Proinflammatory cytokines, such as TNF and IL-1, lead to increased
were higher than in controls without anemia but half that of control iron content in the monocyte/macrophage with induced ferritin
subjects with iron deficiency anemia. During inflammation, EPO expression. The net result is serum hypoferremia and hyperferri-
expression is decreased or inappropriately low for the degree of tinemia. Rats injected with IL-1 or TNF experienced a 40% drop
anemia, which is in part because of cytokine-mediated alterations in serum iron levels; further, TNF also caused a significant decrease
in binding affinities of EPO-inducing transcription factors and to in iron incorporation into erythrocytes. Animals injected with IL-6
damage of EPO-producing cells. For example, LPS injections are have increased hepcidin levels and develop hypoferremia within 24
associated with decreased renal EPO mRNA expression in animal hours, but systemic LPS injection (which leads to IL-6 induction)
models. Similarly, serum EPO levels are inappropriately low in HIV- was not associated with hypoferremia in IL-6 knockout mice. Finally,
positive patients with normochromic, normocytic anemia and in lung TNF has also been shown to increase radiolabeled iron uptake by
transplant recipients. peritoneal macrophages without an increase in iron release, suggest-
Finally, EPO may not function optimally in the presence of inflam- ing that macrophage sequestration of iron is cytokine-induced. All
matory cytokines. EPO-resistant subjects with end-stage renal disease these studies highlight the importance of cytokines in altering iron
(ESRD) are more likely to have elevations in inflammatory cytokines, metabolism in inflammatory situations.
and peripheral blood mononuclear cells isolated from EPO-refractory Molecular evidence implicates both a direct and indirect cytokine
ESRD subjects are more likely to produce inflammatory cytokines effect on iron metabolism. Proinflammatory cytokines IL-1 and IL-6
than are those from non-EPO-refractory ESRD subjects. translationally regulate the expression of ferritin via a 5′ untranslated
region within the ferritin mRNA. This mechanism is distinct from
the iron-responsive element but similar to a 38-nucleotide consensus
BIOLOGY AND MOLECULAR ASPECTS sequence found in other IL-sensitive acute-phase reactants. Since the
increase in ferritin occurs with concomitant downregulation of trans-
The role of inflammatory cytokines in many of the underlying diseases ferrin receptor expression, the mode of cellular iron sequestration is
associated with ACD has suggested a mechanistic link for much of not entirely clear. Hepcidin is a 25-amino acid hepatically derived
the pathophysiology of this anemia, including decreased erythrocyte peptide. Fleming and Sly first suggested a link between hepcidin and
12
survival, decreased access to available iron through upregulation abnormalities in iron metabolism with inflammation. Recent data
of hepcidin, direct inhibition of erythroid progenitor growth, and show that numerous inflammatory cytokines upregulate hepcidin;
inadequate EPO response to anemia. however, experimentally IL-6 and the bone morphogenetic proteins
Increased serum levels of cytokines, particularly IL-1, IL-6, IL-10, (BMPs) are most centrally involved in its synthesis. Hepcidin causes
TNF, IFN-α, IFN-β, and IFN-ɣ, have been observed in many the degradation of ferroportin in duodenal enterocytes and macro-
inflammatory processes, including infections, autoimmune disorders, phages, leading to the decreased gut iron absorption and increased
8
and solid and hematologic malignancies. Often in these disorders, macrophage iron retention that is classically noted with ACD.
cytokine levels frequently inversely correlate with the anemia, so as to The induction of hepcidin expression by inflammation is medi-
13
suggest an association. Serum TNF levels correlate with both disease ated through the transcription factors STAT3 and SMAD4, both
activity and the degree of anemia in RA. Bone marrows from patients of which are upregulated by cytokines via the BMP type I receptors.