Page 1326 - Williams Hematology ( PDFDrive )
P. 1326
1300 Part X: Malignant Myeloid Diseases Chapter 84: Polycythemia Vera 1301
THE SPENT PHASE 1.0
Sometimes after only a few years and usually after 15 years or more, 0.9
erythrocytosis in patients with PV gradually abates in the absence of 0.8
iron deficiency, phlebotomy requirements decrease and cease, and ane- 0.7 N=503
mia develops. During this “spent” phase of the disease, marrow fibrosis 0.6 Medain survival 27.8 years
becomes more marked and the spleen often becomes greatly enlarged Survival 0.5
(see Fig. 84–2A). Instead of phlebotomies, transfusions or erythropoi- 0.4
etin may be required in such patients. The platelet count may remain 0.3
255
high or may decline, even to pronounced thrombocytopenic levels.
N=568
Marked leukopenia or leukocytosis may occur, and immature granulo- 0.2 Median survival 10.9 years N=474
HR 10.7; 95% CI 7.7-15.0
cytes may appear in the blood. At this point, the disease closely mimics 0.1 Median survival 18.9 years
HR 3.7; 95% CI 2.6-5.2
PMF (Chap. 86) and is termed post-PV MF. Treatment of this phase 0.0
of the disease is difficult and requires the judicious use of a combina- 0 10 20 30 40
tion of therapeutic approaches, including HU, erythropoiesis-stimu- Years
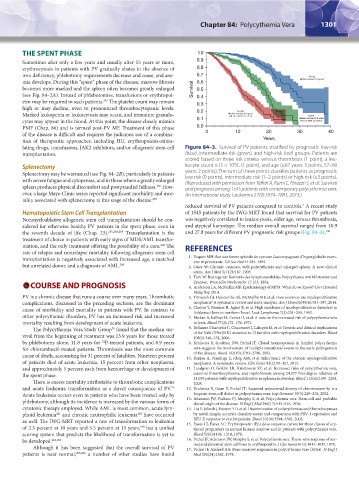
lating drugs, transfusions, JAK2 inhibitors, and/or allogeneic stem cell Figure 84–3. Survival of PV patients stratified by prognostic low-risk
transplantation. (blue), intermediate-risk (green), and high-risk (red) groups. Patients are
scored based on three risk criteria: venous thrombosis (1 point), a leu-
9
Splenectomy kocyte count ≥15 × 10 /L (1 point), and age (≥67 years: 5 points, 57–66
Splenectomy may be warranted (see Fig. 84–2B), particularly in patients years: 2 points). The sum of these points classifies patients as prognostic
with severe fatigue and cytopenias, and in those where a greatly enlarged low risk (0 points), intermediate risk (1–2 points) or high risk (≥3 points).
spleen produces physical discomfort and postprandial fullness. How- (Reproduced with permission from Tefferi A, Rumi E, Finazzi G, et al: Survival
256
and prognosis among 1545 patients with contemporary polycythemia vera:
ever, a large Mayo Clinic series reported significant morbidity and mor- An international study. Leukemia 27(9):1874–1881, 2013.)
tality associated with splenectomy at this stage of the disease. 257
reduced survival of PV patients compared to controls. A recent study
4
Hematopoietic Stem Cell Transplantation of 1545 patients by the IWG-MRT found that survival for PV patients
Nonmyeloablative allogeneic stem cell transplantation should be con- was negatively correlated to leukocytosis, older age, venous thrombosis,
sidered for otherwise healthy PV patients in the spent phase, even in and atypical karyotype. The median overall survival ranged from 10.9
the seventh decade of life (Chap. 23). 255,258,259 Transplantation is the and 27.8 years for different PV prognostic risk groups (Fig. 84–3). 190
treatment of choice in patients with early signs of MDS/AML transfor-
mation, and the only treatment offering the possibility of a cure. The REFERENCES
260
rate of relapse and nonrelapse mortality following allogeneic stem cell
transplantation is negatively associated with increased age, a matched 1. Vaquez MH: Sue une forme spéciale de cyanose s’accompagnant d’hyperglobulie exces-
sive et persistante. CR Soc Biol 44:384, 1892.
but unrelated donor, and a diagnosis of AML. 260 2. Osler W: Chronic cyanosis, with polycythemia and enlarged spleen: A new clinical
entity. Am J Med Sci 126:187, 1903.
3. Türk W: Beitrage zur Kenntnis des Symptomenbildes Polycythamie mit Milztumor und
Zyanose. Wien Klin Wochenschr 17:153, 1904.
COURSE AND PROGNOSIS 4. Anderson LA, McMullin MF: Epidemiology of MPN: What do we know? Curr Hematol
Malig Rep 2014.
PV is a chronic disease that runs a course over many years. Thrombotic 5. Titmarsh GJ, Duncombe AS, McMullin MF, et al: How common are myeloproliferative
complications, discussed in the preceding sections, are the dominant neoplasms? A systematic review and meta-analysis. Am J Hematol 89(6):581–587, 2014.
cause of morbidity and mortality in patients with PV. In contrast to 6. Chaiter Y, Brenner B, Aghai E, et al: High incidence of myeloproliferative disorders in
Ashkenazi Jews in northern Israel. Leuk Lymphoma 7(3):251–255, 1992.
other polycythemic disorders, PV has an increased risk and increased 7. Modan B, Kallner H, Zemer D, et al: A note on the increased risk of polycythemia vera
mortality resulting from development of acute leukemia. in Jews. Blood 37(2):172–176, 1971.
The Polycythemia Vera Study Group found that the median sur- 8. Bellanne-Chantelot C, Chaumarel I, Labopin M, et al: Genetic and clinical implications
76
vival from the beginning of treatment was 13.9 years for those treated of the Val617Phe JAK2 mutation in 72 families with myeloproliferative disorders. Blood
108(1):346–352, 2006.
by phlebotomy alone, 11.8 years for P-treated patients, and 8.9 years 9. Kralovics R, Stockton DW, Prchal JT: Clonal hematopoiesis in familial polycythemia
32
for chlorambucil-treated patients. Thrombosis was the most common vera suggests the involvement of multiple mutational events in the early pathogenesis
of the disease. Blood 102(10):3793–3796, 2003.
cause of death, accounting for 31 percent of fatalities. Nineteen percent 10. Ranjan A, Penninga E, Jelsig AM, et al: Inheritance of the chronic myeloproliferative
of patients died of acute leukemia, 15 percent from other neoplasms, neoplasms. A systematic review. Clin Genet 83(2):99–107, 2013.
and approximately 5 percent each from hemorrhage or development of 11. Landgren O, Goldin LR, Kristinsson SY, et al: Increased risks of polycythemia vera,
the spent phase. essential thrombocythemia, and myelofibrosis among 24,577 first-degree relatives of
There is excess mortality attributable to thrombotic complications 11,039 patients with myeloproliferative neoplasms in Sweden. Blood 112(6):2199–2204,
2008.
and acute leukemia transformation as a direct consequence of PV. 12. Kralovics R, Guan Y, Prchal JT: Acquired uniparental disomy of chromosome 9p is a
75
Acute leukemia occurs even in patients who have been treated only by frequent stem cell defect in polycythemia vera. Exp Hematol 30(3):229–236, 2002.
phlebotomy, although its incidence is increased by the various forms of 13. Adamson JW, Fialkow PJ, Murphy S, et al: Polycythemia vera: Stem-cell and probable
clonal origin of the disease. N Engl J Med 295(17):913–916, 1976.
cytotoxic therapy employed. While AML is most common, acute lym- 14. Liu E, Jelinek J, Pastore YD, et al: Discrimination of polycythemias and thrombocytoses
phoid leukemia and chronic neutrophilic leukemia have occurred by novel, simple, accurate clonality assays and comparison with PRV-1 expression and
261
262
as well. The IWG-MRT reported a rate of transformation to leukemia BFU-E response to erythropoietin. Blood 101(8):3294–3301, 2003.
of 2.3 percent at 10 years and 5.5 percent at 15 years, but a unified 15. Eaves CJ, Eaves AC: Erythropoietin (Ep) dose-response curves for three classes of ery-
190
throid progenitors in normal human marrow and in patients with polycythemia vera.
scoring system that predicts the likelihood of transformation is yet to Blood 52(6):1196–1210, 1978.
be developed. 263,264 16. Prchal JF, Adamson JW, Murphy S, et al: Polycythemia vera. The in vitro response of nor-
mal and abnormal stem cell lines to erythropoietin. J Clin Invest 61(4):1044–1047, 1978.
Although it has been suggested that the overall survival of PV 17. Prchal JF, Axelrad AA: Bone-marrow responses in polycythemia vera [letter]. N Engl J
patients is near normal, 265,266 a number of other studies have found Med 290(24):1382, 1974.
Kaushansky_chapter 84_p1291-1306.indd 1301 9/21/15 11:11 AM