Page 1422 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 1422
CHAPTER 103: Thyroid Disease 995
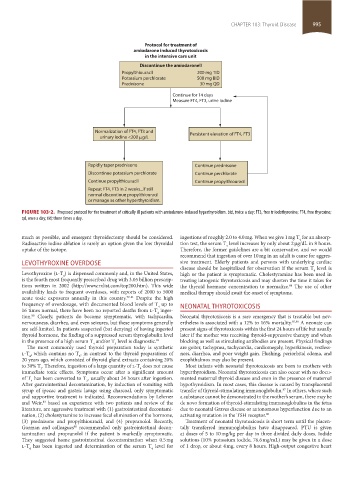
Protocol for treatment of
amiodarone induced thyrotoxicosis
in the intensive care unit
Discontinue the amiodarone!!
Propylthiouracil 200 mg TID
Potassium perchlorate 500 mg BID
Prednisone 30 mg QD
Continue for 14 days
Measure FT4, FT3, urine Iodine
Normalization of FT4, FT3 and Persistent elevation of FT4, FT3
urinary iodine <200 mg/L
Rapidly taper prednisone Continue prednisone
Discontinue potassium perchlorate Continue perchlorate
Continue propylthiouracil Continue propylthiouracil
Repeat FT4, FT3 in 2 weeks...if still
normal discontinue propylthiouracil
or manage as other hyperthyroidism.
FIGURE 103-2. Proposed protocol for the treatment of critically ill patients with amiodarone-induced hyperthyroidism. bid, twice a day; FT3, free triiodothyronine; FT4, free thyroxine;
qd, once a day; tid; three times a day.
much as possible, and emergent thyroidectomy should be considered. ingestions of roughly 2.0 to 4.0 mg. When we give 1 mg T for an absorp-
4
Radioactive iodine ablation is rarely an option given the low thyroidal tion test, the serum T level increases by only about 2 µg/dL in 8 hours.
4
uptake of the isotope. Therefore, the former guidelines are a bit conservative, and we would
recommend that ingestion of over 10 mg in an adult is cause for aggres-
LEvOTHYROXINE OvERDOSE sive treatment. Elderly patients and persons with underlying cardiac
disease should be hospitalized for observation if the serum T level is
4
Levothyroxine (l-T ) is dispensed commonly and, in the United States, high or the patient is symptomatic. Cholestyramine has been used in
4
is the fourth most frequently prescribed drug with 3.05 billion prescrip- treating iatrogenic thyrotoxicosis and may shorten the time it takes for
tions written in 2002 (http://www.rxlist.com/top200.htm). This wide the thyroid hormone concentration to normalize. The use of other
84
availability leads to frequent overdoses, with reports of 2000 to 5000 medical therapy should await the onset of symptoms.
acute toxic exposures annually in this country. 79-81 Despite the high
frequency of overdosage, with documented blood levels of T up to NEONATAL THYROTOXICOSIS
4
16 times normal, there have been no reported deaths from l-T inges-
4
tion. Clearly, patients do become symptomatic, with tachycardia, Neonatal thyrotoxicosis is a rare emergency that is treatable but nev-
80
nervousness, diarrhea, and even seizures, but these symptoms generally ertheless is associated with a 12% to 16% mortality. 85,86 A neonate can
are self-limited. In patients suspected (but denying) of having ingested present signs of thyrotoxicosis within the first 24 hours of life but usually
thyroid hormone, the finding of a suppressed serum thyroglobulin level later if the mother was receiving thyroid-suppressive therapy and when
in the presence of a high serum T and/or T level is diagnostic. 82 blocking as well as stimulating antibodies are present. Physical findings
3
4
The most commonly used thyroid preparation today is synthetic are goiter, tachypnea, tachycardia, cardiomegaly, hyperkinesis, restless-
l-T , which contains no T , in contrast to the thyroid preparations of ness, diarrhea, and poor weight gain. Flushing, periorbital edema, and
4
3
20 years ago, which consisted of thyroid gland extracts containing 20% exophthalmos may also be present.
to 30% T . Therefore, ingestion of a large quantity of l-T does not cause Most infants with neonatal thyrotoxicosis are born to mothers with
4
3
immediate toxic effects. Symptoms occur after a significant amount hyperthyroidism. Neonatal thyrotoxicosis can also occur with no docu-
of T has been converted to T , usually about 24 hours after ingestion. mented maternal thyroid disease and even in the presence of maternal
4
3
After gastrointestinal decontamination, by induction of vomiting with hypothyroidism. In most cases, this disease is caused by transplacental
syrup of ipecac and gastric lavage using charcoal, only symptomatic transfer of thyroid-stimulating immunoglobulin. In others, where such
87
and supportive treatment is indicated. Recommendations by Lehrner a substance cannot be demonstrated in the mother’s serum, there may be
and Weir, based on experience with two patients and review of the de novo formation of thyroid-stimulating immunoglobulins in the fetus
83
literature, are aggressive treatment with (1) gastrointestinal decontami- due to neonatal Graves disease or autonomous hyperfunction due to an
nation, (2) cholestyramine to increase fecal elimination of the hormone, activating mutation in the TSH receptor. 88
(3) prednisone and propylthiouracil, and (4) propranolol. Recently, Treatment of neonatal thyrotoxicosis is short term until the placen-
Gorman and colleagues recommended only gastrointestinal decon- tally transferred immunoglobulins have disappeared. PTU is given
80
tamination and propranolol if the patient is markedly symptomatic. at doses of 5 to 10 mg/kg per day in three divided daily doses. Iodide
They suggested home gastrointestinal decontamination when 0.5 mg solutions (10% potassium iodide, 76.6 mg/mL) may be given in a dose
l-T has been ingested and determination of the serum T level for of 1 drop, or about 4 mg, every 8 hours. High-output congestive heart
4 4
section08.indd 995 1/14/2015 8:28:38 AM