Page 93 - ANUAL REPORT MOH 2017
P. 93
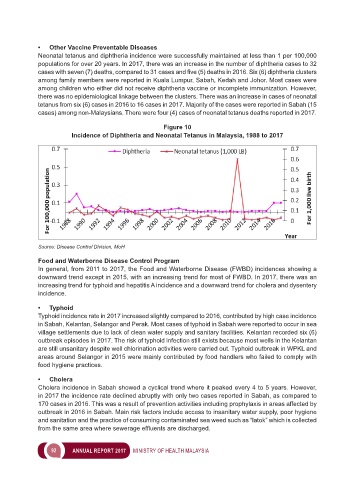
• Other Vaccine Preventable Diseases
Neonatal tetanus and diphtheria incidence were successfully maintained at less than 1 per 100,000
populations for over 20 years. In 2017, there was an increase in the number of diphtheria cases to 32
cases with seven (7) deaths, compared to 31 cases and five (5) deaths in 2016. Six (6) diphtheria clusters
among family members were reported in Kuala Lumpur, Sabah, Kedah and Johor. Most cases were
among children who either did not receive diphtheria vaccine or incomplete immunization. However,
there was no epidemiological linkage between the clusters. There was an increase in cases of neonatal
tetanus from six (6) cases in 2016 to 16 cases in 2017. Majority of the cases were reported in Sabah (15
cases) among non-Malaysians. There were four (4) cases of neonatal tetanus deaths reported in 2017.
Figure 10
Incidence of Diphtheria and Neonatal Tetanus in Malaysia, 1988 to 2017
Source: Disease Control Division, MoH
Food and Waterborne Disease Control Program
In general, from 2011 to 2017, the Food and Waterborne Disease (FWBD) incidences showing a
downward trend except in 2015, with an increasing trend for most of FWBD. In 2017, there was an
increasing trend for typhoid and hepatitis A incidence and a downward trend for cholera and dysentery
incidence.
• Typhoid
Typhoid incidence rate in 2017 increased slightly compared to 2016, contributed by high case incidence
in Sabah, Kelantan, Selangor and Perak. Most cases of typhoid in Sabah were reported to occur in sea
village settlements due to lack of clean water supply and sanitary facilities. Kelantan recorded six (6)
outbreak episodes in 2017. The risk of typhoid infection still exists because most wells in the Kelantan
are still unsanitary despite well chlorination activities were carried out. Typhoid outbreak in WPKL and
areas around Selangor in 2015 were mainly contributed by food handlers who failed to comply with
food hygiene practices.
• Cholera
Cholera incidence in Sabah showed a cyclical trend where it peaked every 4 to 5 years. However,
in 2017 the incidence rate declined abruptly with only two cases reported in Sabah, as compared to
170 cases in 2016. This was a result of prevention activities including prophylaxis in areas affected by
outbreak in 2016 in Sabah. Main risk factors include access to insanitary water supply, poor hygiene
and sanitation and the practice of consuming contaminated sea weed such as “latok” which is collected
from the same area where sewerage effluents are discharged.
92 ANNUAL REPORT 2017 MINISTRY OF HEALTH MALAYSIA