Page 1120 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 1120
CHAPTER 82: Delirium in the Intensive Care Unit 759
Medications
Medications Medical illness
Alcohol withdrawal
Medications Surgical illness
Stroke
Benzodiazepine and
Cholinergic Cholinergic alcohol withdrawal
activation inhibition
Dopamine Reduced
activation GABA activity
https://kat.cr/user/tahir99/
Cytokine GABA Benzodiazepines
excess
activation Hepatic failure
Serotonin Delirium
activation
Glutamate
activation
Serotonin Cortisol
deficiency
excess
Medications
substance withdrawal Tryptophan depletion Hepatic failure
Phenyalanine elevation Alcohol withdrawal
Glucocorticoids
Cushings syndrome
Surgical illness Surgery
Medical illness Stroke
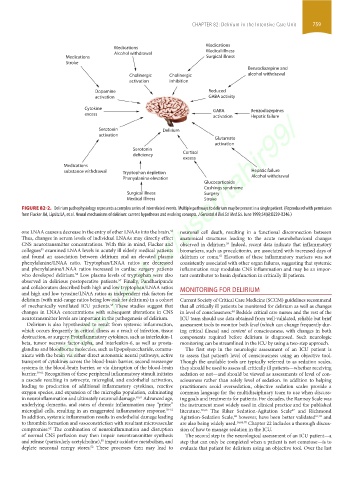
FIGURE 82-2. Delirium pathophysiology represents a complex series of interrelated events. Multiple pathways to delirium may be present in a single patient. (Reproduced with permission
from Flacker JM, Lipsitz LA, et al. Neural mechanisms of delirium: current hypotheses and evolving concepts. J Gerontol A Biol Sci Med Sci. June 1999;54(6):B239-B246.)
one LNAA causes a decrease in the entry of other LNAAs into the brain. neuronal cell death, resulting in a functional disconnection between
52
Thus, changes in serum levels of individual LNAAs may directly effect anatomical structures leading to the acute neurobehavioral changes
CNS neurotransmitter concentrations. With this in mind, Flacker and observed in delirium. Indeed, recent data indicate that inflammatory
59
55
collegues examined LNAA levels in acutely ill elderly medical patients biomarkers, such as procalcitonin, are associated with increased days of
and found an association between delirium and an elevated plasma delirium or coma. Elevation of these inflammatory markers was not
63
phenylalanine/LNAA ratio. Tryptophan/LNAA ratios are decreased consistently associated with other organ failures, suggesting that systemic
and phenylalanine/LNAA ratios increased in cardiac surgery patients inflammation may modulate CNS inflammation and may be an impor-
56
who developed delirium. Low plasma levels of tryptophan were also tant contributor to brain dysfunction in critically ill patients.
observed in delirious postoperative patients. Finally, Pandharipande
57
and collaborators described both high and low tryptophan/LNAA ratios MONITORING FOR DELIRIUM
and high and low tyrosine/LNAA ratios as independent risk factors for
delirium (with mid-range ratios being low-risk for delirium) in a cohort Current Society of Critical Care Medicine (SCCM) guidelines recommend
of mechanically ventilated ICU patients. These studies suggest that that all critically ill patients be monitored for delirium as well as changes
58
changes in LNAA concentrations with subsequent alterations in CNS in level of consciousness. Bedside critical care nurses and the rest of the
64
neurotransmitter levels are important in the pathogenesis of delirium. ICU team should use data obtained from well-validated, reliable but brief
Delirium is also hypothesized to result from systemic inflammation, assessment tools to monitor both level (which can change frequently dur-
which occurs frequently in critical illness as a result of infection, tissue ing critical illness) and content of consciousness, with changes in both
destruction, or surgery. Proinflammatory cytokines, such as interleukin-1 components required before delirium is diagnosed. Such neurologic
beta, tumor necrosis factor-alpha, and interleukin-6, as well as prosta- monitoring can be streamlined in the ICU by using a two-step approach.
glandins and bloodborne molecules, such as lipopolysaccharide, commu- The first step in the neurologic assessment of an ICU patient is
nicate with the brain via either direct autonomic neural pathways, active to assess that patient’s level of consciousness using an objective tool.
transport of cytokines across the blood-brain barrier, second messenger Though the available tools are typically referred to as sedation scales,
systems in the blood-brain barrier, or via disruption of the blood-brain they should be used to assess all critically ill patients—whether receiving
barrier. 59-61 Recognition of these peripheral inflammatory stimuli initiates sedation or not—and should be viewed as assessments of level of con-
a cascade resulting in astrocyte, microglial, and endothelial activation, sciousness rather than solely level of sedation. In addition to helping
leading to production of additional inflammatory cytokines, reactive practitioners avoid oversedation, objective sedation scales provide a
oxygen species, and expansion of the microglia population, culminating common language for the multidisciplinary team to use when discuss-
in neuroinflammation and ultimately neuronal damage. 59,61 Advanced age, ing goals and treatments for patients. For decades, the Ramsay Scale was
underlying dementia, and states of chronic inflammation may “prime” the instrument most widely used in clinical practice and the published
microglial cells, resulting in an exaggerated inflammatory response. 59-61 literature. 65,66 The Riker Sedation-Agitation Scale and Richmond
67
In addition, systemic inflammation results in endothelial damage leading Agitation-Sedation Scale, however, have been better validated 67,69 and
68
to thrombin formation and vasoconstriction with resultant microvascular are also being widely used. 16,66,70 Chapter 22 includes a thorough discus-
compromise. The combination of neuroinflammation and disruption sion of how to manage sedation in the ICU.
62
of normal CNS perfusion may then impair neurotransmitter synthesis The second step in the neurological assessment of an ICU patient—a
and release (particularly acetylcholine), impair oxidative metabolism, and step that can only be completed when a patient is not comatose—is to
50
52
deplete neuronal energy stores. These processes then may lead to evaluate that patient for delirium using an objective tool. Over the last
section06.indd 759 1/23/2015 12:55:27 PM