Page 124 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 124
90 PART 1: An Overview of the Approach to and Organization of Critical Care
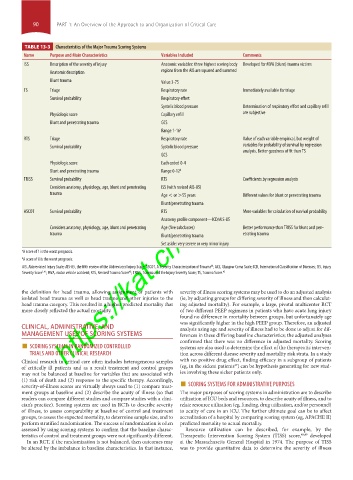
TABLE 13-3 Characteristics of the Major Trauma Scoring Systems
Name Purpose and Main Characteristics Variables Included Comments
ISS Description of the severity of injury Anatomic variables: three highest scoring body Developed for MVA (blunt) trauma victims
Anatomic description regions from the AIS are squared and summed
Blunt trauma Value 3-75
TS Triage Respiratory rate Immediately available for triage
Survival probability Respiratory effort
Systolic blood pressure Determination of respiratory effort and capillary refill
Physiologic score Capillary refill are subjective
Blunt and penetrating trauma GCS
Range 1-16 a
RTS Triage Respiratory rate Value of each variable empirical, but weight of
Survival probability Systolic blood pressure variables for probability of survival by regression
analysis. Better goodness of fit than TS
GCS
Physiologic score Each coded 0-4
Blunt and penetrating trauma Range 0-12 b
TRISS Survival probability RTS Coefficients by regression analysis
Considers anatomy, physiology, age, blunt and penetrating ISS (with revised AIS-85)
trauma Age < or >55 years Different values for blunt or penetrating trauma
Blunt/penetrating trauma
ASCOT Survival probability RTS More variables for calculation of survival probability
Anatomy profile component—ICD/AIS-85
Considers anatomy, physiology, age, blunt and penetrating Age (five subclasses) Better performance than TRISS for blunt and pen-
etrating trauma
trauma https://kat.cr/user/tahir99/
Blunt/penetrating trauma
Set aside: very severe or very minor injury
a A score of 1 is the worst prognosis.
b A score of 0 is the worst prognosis.
AIS, Abbreviated Injury Scale; AIS-85, the fifth review of the Abbreviated Injury Scale; ASCOT, A Severity Characterization of Trauma ; GCS, Glasgow Coma Scale; ICD, International Classification of Diseases; ISS, Injury
44
1,41
43
Severity Score ; MVA, motor vehicle accident; RTS, Revised Trauma Score ; TRISS, Trauma and the Injury Severity Score; TS, Trauma Score. 42
the definition for head trauma, allowing assignment of patients with severity of illness scoring systems may be used to do an adjusted analysis
isolated head trauma as well as head trauma and other injuries to the (ie, by adjusting groups for differing severity of illness and then calculat-
head trauma category. This resulted in a higher predicted mortality that ing adjusted mortality). For example, a large, pivotal multicenter RCT
more closely reflected the actual mortality. of two different PEEP regimens in patients who have acute lung injury
found no difference in mortality between groups, but unfortunately age
was significantly higher in the high PEEP group. Therefore, an adjusted
CLINICAL, ADMINISTRATIVE, AND analysis using age and severity of illness had to be done to adjust for dif-
MANAGEMENT USES OF SCORING SYSTEMS ferences in these differing baseline characteristics; the adjusted analyses
■ SCORING SYSTEMS IN RANDOMIZED CONTROLLED confirmed that there was no difference in adjusted mortality. Scoring
systems are also used to determine the effect of the therapeutic interven-
TRIALS AND OTHER CLINICAL RESEARCH tion across different disease severity and mortality risk strata. In a study
Clinical research in critical care often includes heterogeneous samples with no positive drug effect, finding efficacy in a subgroup of patients
47
of critically ill patients and as a result treatment and control groups (eg, in the sickest patients ) can be hypothesis generating for new stud-
may not be balanced at baseline for variables that are associated with ies involving these sicker patients only.
severity-of-illness scores are virtually always used to (1) compare treat- ■ SCORING SYSTEMS FOR ADMINISTRATIVE PURPOSES
(1) risk of death and (2) response to the specific therapy. Accordingly,
ment groups at baseline and (2) describe the acuity of illness (so that The major purposes of scoring systems in administration are to describe
readers can compare different studies and compare studies with a clini- utilization of ICU beds and resources, to describe acuity of illness, and to
cian’s practice). Scoring systems are used in RCTs to describe severity relate resource utilization (eg, funding, drug utilization, and/or personnel)
of illness, to assess comparability at baseline of control and treatment to acuity of care in an ICU. The further ultimate goal can be to affect
groups, to assess the expected mortality, to determine sample size, and to accreditation of a hospital by comparing scoring system (eg, APACHE II)
perform stratified randomization. The success of randomization is often predicted mortality to actual mortality.
assessed by using scoring systems to confirm that the baseline charac- Resource utilization can be described, for example, by the
teristics of control and treatment groups were not significantly different. Therapeutic Intervention Scoring System (TISS) score, 48,49 developed
In an RCT, if the randomization is not balanced, then outcomes may at the Massachusetts General Hospital in 1974. The purpose of TISS
be altered by the imbalance in baseline characteristics. In that instance, was to provide quantitative data to determine the severity of illness
Section01.indd 90 1/22/2015 9:37:26 AM