Page 667 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 667
486 PART 4: Pulmonary Disorders
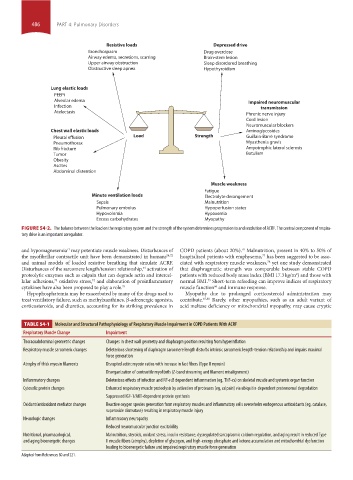
Resistive loads Depressed drive
Bronchospasm Drug overdose
Airway edema, secretions, scarring Brain-stem lesion
Upper airway obstruction Sleep disordered breathing
Obstructive sleep apnea Hypothyroidism
Lung elastic loads
PEEPi
Alveolar edema Impaired neuromuscular
Infection transmission
Atelectasis
Phrenic nerve injury
Cord lesion
Neuromuscular blockers
Chest wall elastic loads Aminoglycosides
Pleural effusion Load Strength Guillain-Barré syndrome
Pneumothorax Myasthenia gravis
Rib fracture Amyotrophic lateral sclerosis
Tumor Botulism
Obesity
Ascites
Abdominal distention
Muscle weakness
Fatigue
Minute ventilation loads Electrolyte derangement
Sepsis Malnutrition
Pulmonary embolus Hypoperfusion states
Hypovolemia Hypoxemia
Excess carbohydrates Myopathy
FIGURE 54-2. The balance between the load on the respiratory system and the strength of the system determines progression to and resolution of ACRF. The central component of respira-
tory drive is an important coregulator.
71
76
and hypomagnesemia may potentiate muscle weakness. Disturbances of COPD patients (about 20%). Malnutrition, present in 40% to 50% of
the myofibrillar contractile unit have been demonstrated in humans 54,72 hospitalized patients with emphysema, has been suggested to be asso-
77
and animal models of loaded resistive breathing that simulate ACRF. ciated with respiratory muscle weakness, yet one study demonstrated
78
Disturbances of the sarcomere length/tension relationship, activation of that diaphragmatic strength was comparable between stable COPD
54
2
proteolytic enzymes such as calpain that can degrade actin and intercel- patients with reduced body mass index (BMI 17.3 kg/m ) and those with
lular adhesions, oxidative stress, and elaboration of proinflammatory normal BMI. Short-term refeeding can improve indices of respiratory
74
79
73
66
cytokines have also been proposed to play a role. 75 muscle function and immune response.
Hypophosphatemia may be exacerbated by many of the drugs used to Myopathy due to prolonged corticosteroid administration may
treat ventilatory failure, such as methylxanthines, β-adrenergic agonists, contribute. 67,80 Rarely, other myopathies, such as an adult variant of
corticosteroids, and diuretics, accounting for its striking prevalence in acid maltase deficiency or mitochondrial myopathy, may cause cryptic
TABLE 54-1 Molecular and Structural Pathophysiology of Respiratory Muscle Impairment in COPD Patients With ACRF
Respiratory Muscle Change Impairment
Thoracoabdominal geometric changes Changes in chest wall geometry and diaphragm position resulting from hyperinflation
Respiratory muscle sarcomeric changes Deleterious shortening of diaphragm sarcomere length disturbs intrinsic sarcomeric length-tension relationship and impairs maximal
force generation
Atrophy of thick myosin filaments Disrupted actin: myosin ratios with increase in fast fibers (Type II myosin)
Disorganization of contractile myofibrils (Z-band streaming and filament misalignment)
Inflammatory changes Deleterious effects of infection and NF-κB dependent inflammation (eg, TNF-α) on skeletal muscle and systemic organ function
Cytosolic protein changes Enhanced respiratory muscle proteolysis by activation of proteases (eg, calpain) via ubiquitin-dependent proteosomal degradation
Suppressed IGF-1/AKT-dependent protein synthesis
Oxidant/antioxidant mediator changes Reactive oxygen species generation from respiratory muscles and inflammatory cells overwhelm endogenous antioxidants (eg, catalase,
superoxide dismutase) resulting in respiratory muscle injury
Neurologic changes Inflammatory neuropathy
Reduced neuromuscular junction excitability
Nutritional, pharmacological, Malnutrition, steroids, oxidant stress, insulin resistance, dysregulated sarcoplasmic calcium regulation, and aging result in reduced Type
and aging bioenergetic changes II muscle fibers (atrophy), depletion of glycogen, and high-energy phosphate and ketone accumulation and mitochondrial dysfunction
leading to bioenergetic failure and impaired respiratory muscle force generation
Adapted from References 80 and 221.
section04.indd 486 1/23/2015 2:20:07 PM