Page 833 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 833
564 PART 5: Infectious Disorders
patients with cancer, diabetes, and HIV disease. 6,11,12 Remarkably, patients T-cell stimulation. Gram-negative bacteria, such as Escherichia coli,
14
with cancer have among the highest population-adjusted rates for sepsis— have a complex lipid called lipopolysaccharide (LPS) in its membrane
similarly high to that for patients with HIV and exceeding estimated rates barrier, which activates the innate host immune response. Similar to
15
with chronic lung disease, heart disease, and diabetes. 11 bacteria, viruses have a unique molecular pattern that is recognized
Sepsis incidence and mortality is also influenced by regional, seasonal, and identified by various host Toll-like receptors (TLR). Additionally,
and cultural factors. Sepsis rates are lowest in the fall and highest in an immunosuppressed host can fall prey to fungal infections such as
the winter, with the greatest increase in cases due to respiratory infec- Candida albicans, an opportunistic pathogen that develops as a con-
tion. Regional differences in sepsis incidence are also apparent, with sequence of an inadequate immune host response. It is able to display
higher rates in the Northeastern United States and the greatest seasonal various morphologies from a unicellular form (eg, hyphae, pseudohy-
changes in rates between the fall and winter seasons also seen in the phae, or chlamydospores) and can threaten an altered immune host.
16
Northeast. Both the seasonal and regional variation may relate to As mentioned above, sepsis can occur with any of these microorganisms
13
rates of viral infections, which closely track cases of respiratory sepsis. and each may initiate a host immune response resulting in a complex
Infection and sepsis rates are affected by myriad factors in the develop- inflammatory and coagulation cascade.
ing world, including climatic conditions, and although data outside of
well-developed nations are sparse, the frequency of infectious diseases Host Immune Response: The host’s response to an infection depends
makes sepsis a likely culprit for the leading cause of death worldwide. on both the innate and acquired host immune system. Certain
patients are more susceptible to sepsis due to their inability to mount
a normal immune response. The first line of host defense is the epi-
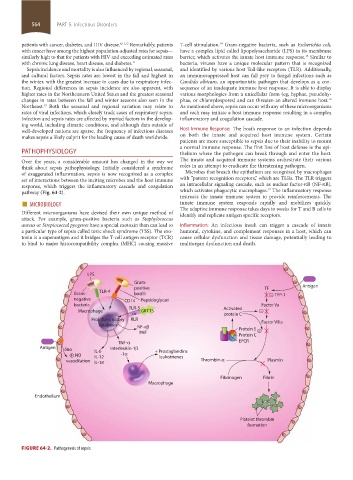
PATHOPHYSIOLOGY thelium where the pathogen can break through and enter the host.
Over the years, a considerable amount has changed in the way we The innate and acquired immune systems orchestrate their various
think about sepsis pathophysiology. Initially considered a syndrome roles in an attempt to eradicate the threatening pathogen.
of exaggerated inflammation, sepsis is now recognized as a complex Microbes that breach the epithelium are recognized by macrophages
set of interactions between the inciting microbes and the host immune with “pattern recognition receptors,” which are TLRs. The TLR triggers
response, which triggers the inflammatory cascade and coagulation an intracellular signaling cascade, such as nuclear factor-κB (NF-κB),
17
pathway (Fig. 64-2). which activates phagocytic macrophages. The inflammatory response
■ MICROBIOLOGY innate immune system responds rapidly and mobilizes quickly.
instructs the innate immune system to provide reinforcements. The
Different microorganisms have devised their own unique method of The adaptive immune response takes days to weeks for T and B cells to
identify and replicate antigen specific receptors.
attack. For example, gram-positive bacteria such as Staphylococcus
aureus or Streptococcal pyogenes have a special exotoxin than can lead to Inflammation: An infectious insult can trigger a cascade of innate
a particular type of sepsis called toxic shock syndrome (TSS). The exo- humoral, cytokine, and complement responses in a host, which can
toxin is a superantigen and it bridges the T-cell antigen receptor (TCR) cause cellular dysfunction and tissue damage, potentially leading to
to bind to major histocompatibility complex (MHC) causing massive multiorgan dysfunction and death.
LPS
Gram-
positive TF Antigen
Gram- TLR-4 bacilli – TFP-1
negative CD14 Peptidoglycan
bacteria TLR-3 Factor Va
Macrophage GKTTS Activated –
or protein C
Proinflammatory RLR Factor VIIIa
cytokines NF-
PAF Protein S –
Protein C
TNF- EPCR
Antigen Interleukin-1
no IL-6 + Prostaglandins
+ NO IL-12 -1 leukotrienes
vasodilation IL-18 Thrombin- Plasmin
Fibrinogen Fibrin
Macrophage
Endothelium
Platelet thrombin
formation
FIGURE 64-2. Pathogenesis of sepsis.
section05_c61-73.indd 564 1/23/2015 12:47:49 PM