Page 832 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 832
CHAPTER 64: Sepsis, Severe Sepsis, and Septic Shock 563
developed two new and important concepts. The first concept is that the
TABLE 64-1 Definition of Sepsis and Related Disorders
SIRS criteria are only a few signs or symptoms that may indicate sepsis,
Disease State Definition Mortality and while a new version of the SIRS criteria was not proposed, it was
Sepsis Infection + at least two SIRS criteria Determined by the recognized that delaying a diagnosis of sepsis when the traditional four
underlying condition SIRS criteria are absent is ultimately a disservice to an acute ill patient.
Additional potential criteria were proposed, including heterogeneous
Severe sepsis Sepsis with acute organ dysfunction 25%-40%
clinical and laboratory manifestations of systemic illness (alterations
Septic shock Sepsis with refractory hypotension despite 40%-80% in mental status or hyperglycemia), infection (eg, elevated C-reactive
adequate fluid loading (vasoplegia) protein or procalcitonin), and even sepsis-related organ dysfunction
(central venous hypoxia, coagulopathy, oliguria, mottling). The second
important concept put forth was the necessity to characterize the “stage”
trials and test new therapeutics. Although the ACCP/SCCM consen- of illness for sepsis patients, as is done with cancer or heart disease. They
sus definition is imperfect, suffering from both a lack of sensitivity proposed this as the PIRO model—Predisposition, Insult/Infection,
and specificity, it has transformed our understanding of sepsis epidemi- Response, Organ dysfunction—which has since been validated as a tool
ology and pathogenesis, and it has permitted the successful testing of for prognosticating outcomes with sepsis. 2-4
novel therapies for this condition.
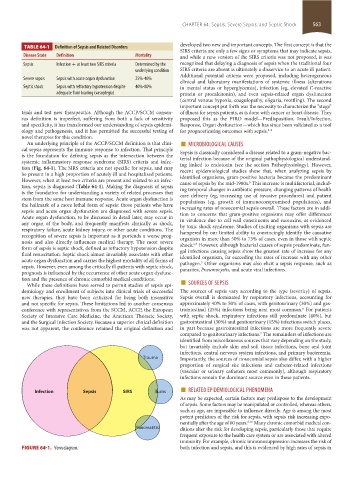
An underlying principle of the ACCP/SCCM definition is that clini- ■ MICROBIOLOGICAL CAUSES
cal sepsis represents the immune response to infection. That principle Sepsis is classically considered a disease related to a gram-negative bac-
is the foundation for defining sepsis as the intersection between the terial infection because of the original pathophysiological understand-
systemic inflammatory response syndrome (SIRS) criteria and infec- ing linked to endotoxin (see the section Pathophysiology). However,
tion (Fig. 64-1). The SIRS criteria are not specific for sepsis, and may recent epidemiological studies show that, when analyzing sepsis by
be present in a high proportion of acutely ill and hospitalized patients. identified organisms, gram-positive bacteria became the predominant
However, when at least two criteria are present and related to an infec- cause of sepsis by the mid-1980s. This increase is multifactorial, includ-
5
tion, sepsis is diagnosed (Table 64-1). Making the diagnosis of sepsis ing temporal changes in antibiotic pressure, changing patterns of health
is the foundation for understanding a variety of related processes that care delivery (eg, increasing use of invasive procedures) and patient
stem from the same host immune response. Acute organ dysfunction is populations (eg, growth of immunocompromised populations), and
the hallmark of a more lethal form of sepsis: those patients who have increasing rates of nosocomial sepsis overall. These factors are in addi-
sepsis and acute organ dysfunction are diagnosed with severe sepsis. tion to concerns that gram-positive organisms may offer differences
Acute organ dysfunction, to be discussed in detail later, may occur in in virulence due to cell wall constituents and exotoxins, as evidenced
any organ of the body, and frequently manifests clinically as shock, by toxic shock syndrome. Studies of inciting organisms with sepsis are
respiratory failure, acute kidney injury, or other acute conditions. The hampered by our limited ability to convincingly identify the causative
recognition of severe sepsis is important as it portends a worse prog- organism in more than 50% to 75% of cases, even in those with septic
nosis and also directly influences medical therapy. The most severe shock. However, although bacterial causes of sepsis predominate, fun-
6,7
form of sepsis is septic shock, defined as refractory hypotension despite gal infections causing sepsis show the greatest rate of increase for any
fluid resuscitation. Septic shock almost invariably associates with other identified organism, far exceeding the rates of increase with any other
acute organ dysfunction and carries the highest mortality of all forms of pathogen. Other organisms may also elicit a sepsis response, such as
5
sepsis. However, even among the critically ill patients with septic shock, parasites, Pneumocystis, and acute viral infections.
prognosis is influenced by the occurrence of other acute organ dysfunc-
While these definitions have served to permit studies of sepsis epi- ■
tion and the presence of chronic comorbid medical conditions. SOURCES OF SEPSIS
demiology and enrollment of subjects into clinical trials of successful The sources of sepsis vary according to the type (severity) of sepsis.
new therapies, they have been criticized for being both insensitive Sepsis overall is dominated by respiratory infections, accounting for
and not specific for sepsis. These limitations led to another consensus approximately 40% to 50% of cases, with genitourinary (30%) and gas-
conference with representatives from the SCCM, ACCP, the European trointestinal (25%) infections being next most common. For patients
6
Society of Intensive Care Medicine, the American Thoracic Society, with septic shock, respiratory infections still predominate (40%), but
and the Surgical Infection Society. Because a superior clinical definition gastrointestinal (30%) and genitourinary (15%) infections switch places,
was not apparent, the conference retained the original definition and in part because gastrointestinal infections are more frequently severe
compared to genitourinary infections. The remainders of infections are
7
identified from miscellaneous sources that vary depending on the study,
but invariably include skin and soft tissue infections, bone and joint
infections, central nervous system infections, and primary bacteremia.
Trauma Importantly, the sources of nosocomial sepsis also differ, with a higher
proportion of surgical site infections and catheter-related infections
(vascular or urinary catheters most commonly), although respiratory
infections remain the dominant source even in these patients.
Burns ■
Infection Sepsis SIRS RELATED EPIDEMIOLOGICAL PHENOMENA
As may be expected, certain factors may predispose to the development
of sepsis. Some factors may be manipulated or controlled, whereas others,
such as age, are impossible to influence directly. Age is among the most
potent predictors of the risk for sepsis, with sepsis risk increasing expo-
nentially after the age of 60 years. 8-10 Many chronic comorbid medical con-
Pancreatitis ditions alter the risk for developing sepsis, particularly those that require
frequent exposure to the health care system or are associated with altered
immunity. For example, chronic immunosuppression increases the risk of
FIGURE 64-1. Venn diagram. both infection and sepsis, and this is evidenced by high rates of sepsis in
section05_c61-73.indd 563 1/23/2015 12:47:21 PM