Page 119 - Critical Care Notes
P. 119
4223_Tab03_107-130 29/08/14 8:28 AM Page 113
113
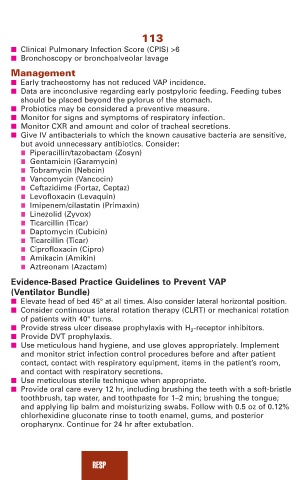
■ Clinical Pulmonary Infection Score (CPIS) >6
■ Bronchoscopy or bronchoalveolar lavage
Management
■ Early tracheostomy has not reduced VAP incidence.
■ Data are inconclusive regarding early postpyloric feeding. Feeding tubes
should be placed beyond the pylorus of the stomach.
■ Probiotics may be considered a preventive measure.
■ Monitor for signs and symptoms of respiratory infection.
■ Monitor CXR and amount and color of tracheal secretions.
■ Give IV antibacterials to which the known causative bacteria are sensitive,
but avoid unnecessary antibiotics. Consider:
■ Piperacillin/tazobactam (Zosyn)
■ Gentamicin (Garamycin)
■ Tobramycin (Nebcin)
■ Vancomycin (Vancocin)
■ Ceftazidime (Fortaz, Ceptaz)
■ Levofloxacin (Levaquin)
■ Imipenem/cilastatin (Primaxin)
■ Linezolid (Zyvox)
■ Ticarcillin (Ticar)
■ Daptomycin (Cubicin)
■ Ticarcillin (Ticar)
■ Ciprofloxacin (Cipro)
■ Amikacin (Amikin)
■ Aztreonam (Azactam)
Evidence-Based Practice Guidelines to Prevent VAP
(Ventilator Bundle)
■ Elevate head of bed 45° at all times. Also consider lateral horizontal position.
■ Consider continuous lateral rotation therapy (CLRT) or mechanical rotation
of patients with 40° turns.
■ Provide stress ulcer disease prophylaxis with H 2 -receptor inhibitors.
■ Provide DVT prophylaxis.
■ Use meticulous hand hygiene, and use gloves appropriately. Implement
and monitor strict infection control procedures before and after patient
contact, contact with respiratory equipment, items in the patient’s room,
and contact with respiratory secretions.
■ Use meticulous sterile technique when appropriate.
■ Provide oral care every 12 hr, including brushing the teeth with a soft-bristle
toothbrush, tap water, and toothpaste for 1–2 min; brushing the tongue;
and applying lip balm and moisturizing swabs. Follow with 0.5 oz of 0.12%
chlorhexidine gluconate rinse to tooth enamel, gums, and posterior
oropharynx. Continue for 24 hr after extubation.
RESP