Page 124 - Critical Care Notes
P. 124
4223_Tab03_107-130 29/08/14 8:28 AM Page 118
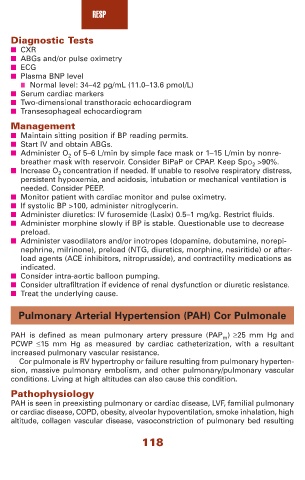
RESP
Diagnostic Tests
■ CXR
■ ABGs and/or pulse oximetry
■ ECG
■ Plasma BNP level
■ Normal level: 34–42 pg/mL (11.0–13.6 pmol/L)
■ Serum cardiac markers
■ Two-dimensional transthoracic echocardiogram
■ Transesophageal echocardiogram
Management
■ Maintain sitting position if BP reading permits.
■ Start IV and obtain ABGs.
■ Administer O 2 of 5–6 L/min by simple face mask or 1–15 L/min by nonre-
breather mask with reservoir. Consider BiPaP or CPAP. Keep SpO 2 >90%.
■ Increase O 2 concentration if needed. If unable to resolve respiratory distress,
persistent hypoxemia, and acidosis, intubation or mechanical ventilation is
needed. Consider PEEP.
■ Monitor patient with cardiac monitor and pulse oximetry.
■ If systolic BP >100, administer nitroglycerin.
■ Administer diuretics: IV furosemide (Lasix) 0.5–1 mg/kg. Restrict fluids.
■ Administer morphine slowly if BP is stable. Questionable use to decrease
preload.
■ Administer vasodilators and/or inotropes (dopamine, dobutamine, norepi-
nephrine, milrinone), preload (NTG, diuretics, morphine, nesiritide) or after-
load agents (ACE inhibitors, nitroprusside), and contractility medications as
indicated.
■ Consider intra-aortic balloon pumping.
■ Consider ultrafiltration if evidence of renal dysfunction or diuretic resistance.
■ Treat the underlying cause.
Pulmonary Arterial Hypertension (PAH) Cor Pulmonale
PAH is defined as mean pulmonary artery pressure (PAP m ) ≥25 mm Hg and
PCWP ≤15 mm Hg as measured by cardiac catheterization, with a resultant
increased pulmonary vascular resistance.
Cor pulmonale is RV hypertrophy or failure resulting from pulmonary hyperten-
sion, massive pulmonary embolism, and other pulmonary/pulmonary vascular
conditions. Living at high altitudes can also cause this condition.
Pathophysiology
PAH is seen in preexisting pulmonary or cardiac disease, LVF, familial pulmonary
or cardiac disease, COPD, obesity, alveolar hypoventilation, smoke inhalation, high
altitude, collagen vascular disease, vasoconstriction of pulmonary bed resulting
118