Page 122 - Critical Care Notes
P. 122
4223_Tab03_107-130 29/08/14 8:28 AM Page 116
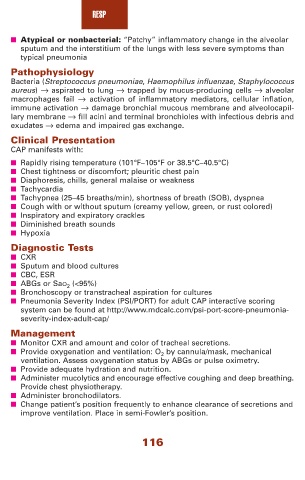
RESP
■ Atypical or nonbacterial: “Patchy” inflammatory change in the alveolar
sputum and the interstitium of the lungs with less severe symptoms than
typical pneumonia
Pathophysiology
Bacteria (Streptococcus pneumoniae, Haemophilus influenzae, Staphylococcus
aureus) → aspirated to lung → trapped by mucus-producing cells → alveolar
macrophages fail → activation of inflammatory mediators, cellular inflation,
immune activation → damage bronchial mucous membrane and alveolocapil-
lary membrane → fill acini and terminal bronchioles with infectious debris and
exudates → edema and impaired gas exchange.
Clinical Presentation
CAP manifests with:
■ Rapidly rising temperature (101°F–105°F or 38.5°C–40.5°C)
■ Chest tightness or discomfort; pleuritic chest pain
■ Diaphoresis, chills, general malaise or weakness
■ Tachycardia
■ Tachypnea (25–45 breaths/min), shortness of breath (SOB), dyspnea
■ Cough with or without sputum (creamy yellow, green, or rust colored)
■ Inspiratory and expiratory crackles
■ Diminished breath sounds
■ Hypoxia
Diagnostic Tests
■ CXR
■ Sputum and blood cultures
■ CBC, ESR
■ ABGs or SaO 2 (<95%)
■ Bronchoscopy or transtracheal aspiration for cultures
■ Pneumonia Severity Index (PSI/PORT) for adult CAP interactive scoring
system can be found at http://www.mdcalc.com/psi-port-score-pneumonia-
severity-index-adult-cap/
Management
■ Monitor CXR and amount and color of tracheal secretions.
■ Provide oxygenation and ventilation: O 2 by cannula/mask, mechanical
ventilation. Assess oxygenation status by ABGs or pulse oximetry.
■ Provide adequate hydration and nutrition.
■ Administer mucolytics and encourage effective coughing and deep breathing.
Provide chest physiotherapy.
■ Administer bronchodilators.
■ Change patient’s position frequently to enhance clearance of secretions and
improve ventilation. Place in semi-Fowler’s position.
116