Page 164 - Critical Care Notes
P. 164
4223_Tab05_141-174 29/08/14 8:28 AM Page 158
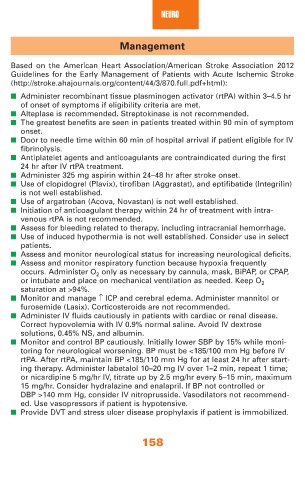
NEURO
Management
Based on the American Heart Association/American Stroke Association 2012
Guidelines for the Early Management of Patients with Acute Ischemic Stroke
(http://stroke.ahajournals.org/content/44/3/870.full.pdf+html):
■ Administer recombinant tissue plasminogen activator (rtPA) within 3–4.5 hr
of onset of symptoms if eligibility criteria are met.
■ Alteplase is recommended. Streptokinase is not recommended.
■ The greatest benefits are seen in patients treated within 90 min of symptom
onset.
■ Door to needle time within 60 min of hospital arrival if patient eligible for IV
fibrinolysis.
■ Antiplatelet agents and anticoagulants are contraindicated during the first
24 hr after IV rtPA treatment.
■ Administer 325 mg aspirin within 24–48 hr after stroke onset.
■ Use of clopidogrel (Plavix), tirofiban (Aggrastat), and eptifibatide (Integrilin)
is not well established.
■ Use of argatroban (Acova, Novastan) is not well established.
■ Initiation of anticoagulant therapy within 24 hr of treatment with intra-
venous rtPA is not recommended.
■ Assess for bleeding related to therapy, including intracranial hemorrhage.
■ Use of induced hypothermia is not well established. Consider use in select
patients.
■ Assess and monitor neurological status for increasing neurological deficits.
■ Assess and monitor respiratory function because hypoxia frequently
occurs. Administer O 2 only as necessary by cannula, mask, BiPAP, or CPAP,
or intubate and place on mechanical ventilation as needed. Keep O 2
saturation at >94%.
■ Monitor and manage ↑ ICP and cerebral edema. Administer mannitol or
furosemide (Lasix). Corticosteroids are not recommended.
■ Administer IV fluids cautiously in patients with cardiac or renal disease.
Correct hypovolemia with IV 0.9% normal saline. Avoid IV dextrose
solutions, 0.45% NS, and albumin.
■ Monitor and control BP cautiously. Initially lower SBP by 15% while moni-
toring for neurological worsening. BP must be <185/100 mm Hg before IV
rtPA. After rtPA, maintain BP <185/110 mm Hg for at least 24 hr after start-
ing therapy. Administer labetalol 10–20 mg IV over 1–2 min, repeat 1 time;
or nicardipine 5 mg/hr IV, titrate up by 2.5 mg/hr every 5–15 min, maximum
15 mg/hr. Consider hydralazine and enalapril. If BP not controlled or
DBP >140 mm Hg, consider IV nitroprusside. Vasodilators not recommend-
ed. Use vasopressors if patient is hypotensive.
■ Provide DVT and stress ulcer disease prophylaxis if patient is immobilized.
158