Page 556 - Cardiac Nursing
P. 556
1
1:0
009
1
1:0
M
M
1 A
1 A
009
3
3
xd
xd
3
6/2
6/2
0/0
0/0
M
p
p
A
p
t
ara
ara
t
ara
A
g
g
Pa
Pa
g
32
32
e 5
e 5
0-c
K34
22_
0-c
LWBK340-c22_ p p pp511-536.qxd 30/06/2009 11:01 AM Page 532 Aptara
36.
1-5
K34
36.
1-5
51
51
22_
q
q
q
532 PA R T I V / Pathophysiology and Management of Heart Disease
Pa
e
th
R
th
on
rc
fa
f
V
In
wi
en
en
ti
ti
t
w
wi
wi
n
1
2
2
2
r
e
a
g
C
P
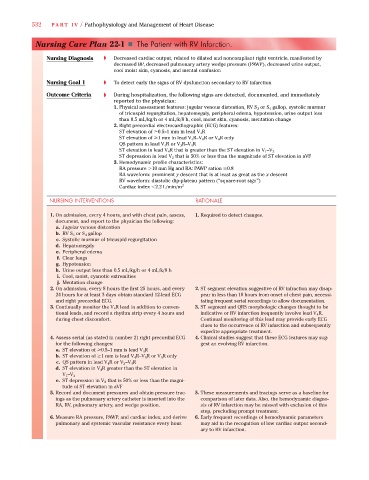
Nursing Care Plan 22-1 Th The PPatientt with RV Infarctiioon.
n
a
l
a
Nursing Diagnosis ➧ Decreased cardiac output, related to dilated and noncompliant right ventricle, manifested by
decreased BP, decreased pulmonary artery wedge pressure (PAWP), decreased urine output,
cool moist skin, cyanosis, and mental confusion
Nursing Goal 1 ➧ To detect early the signs of RV dysfunction secondary to RV infarction
Outcome Criteria ➧ During hospitalization, the following signs are detected, documented, and immediately
reported to the physician:
1. Physical assessment features: jugular venous distention, RV S 3 or S 4 gallop, systolic murmur
of tricuspid regurgitation, hepatomegaly, peripheral edema, hypotension, urine output less
than 0.5 mL/kg/h or 4 mL/k/8 h, cool, moist skin, cyanosis, mentation change
2. Right precordial electrocardiographic (ECG) features:
ST elevation of 0.5–1 mm in lead V 4 R
ST elevation of 1 mm in lead V 4 R–V 6 R or V 6 R only
QS pattern in lead V 4 R or V 3 R–V 4 R
ST elevation in lead V 4 R that is greater than the ST elevation in V 1 –V 3
ST depression in lead V 2 that is 50% or less than the magnitude of ST elevation in aVF
3. Hemodynamic profile characteristics:
RA pressure 10 mm Hg and RA: PAWP ration 0.8
RA waveform: prominent y descent that is at least as great as the x descent
RV waveform: diastolic dip-plateau pattern (“square-root sign”)
Cardiac index 2.2 L/min/m 2
NURSING INTERVENTIONS RATIONALE
1. On admission, every 4 hours, and with chest pain, assess, 1. Required to detect changes.
document, and report to the physician the following:
a. Jugular venous distention
b. RV S 3 or S 4 gallop
c. Systolic murmur of tricuspid regurgitation
d. Hepatomegaly
e. Peripheral edema
f. Clear lungs
g. Hypotension
h. Urine output less than 0.5 mL/kg/h or 4 mL/k/8 h
i. Cool, moist, cyanotic extremities
j. Mentation change
2. On admission, every 8 hours the first 25 hours, and every 2. ST segment elevation suggestive of RV infraction may disap-
24 hours for at least 3 days obtain standard 12-lead ECG pear in less than 10 hours from onset of chest pain, necessi-
and right precordial ECG. tating frequent serial recordings to allow documentation.
3. Continually monitor the V 4 R lead in addition to conven- 3. ST segment and QRS morphologic changes thought to be
tional leads, and record a rhythm strip every 4 hours and indicative or RV infarction frequently involve lead V 4 R.
during chest discomfort. Continual monitoring of this lead may provide early ECG
clues to the occurrence of RV infarction and subsequently
expedite appropriate treatment.
4. Assess serial (as stated in number 2) right precordial ECG 4. Clinical studies suggest that these ECG features may sug-
for the following changes: gest an evolving RV infarction.
a. ST elevation of 0.5–1 mm is lead V 4 R
b. ST elevation of 1 mm is lead V 4 R–V 6 R or V 6 R only
c. QS pattern in lead V 4 R or V 3 –V 4 R
d. ST elevation in V 4 R greater than the ST elevation in
V 1 –V 3
e. ST depression in V 2 that is 50% or less than the magni-
tude of ST elevation in aVF
5. Record and document pressures and obtain pressure trac- 5. These measurements and tracings serve as a baseline for
ings as the pulmonary artery catheter is inserted into the comparison of later data. Also, the hemodynamic diagno-
RA, RV, pulmonary artery, and wedge position. sis of RV infarction may be missed with exclusion of this
step, precluding prompt treatment.
6. Measure RA pressure, PAWP, and cardiac index, and derive 6. Early frequent recordings of hemodynamic parameters
pulmonary and systemic vascular resistance every hour. may aid in the recognition of low cardiac output second-
ary to RV infarction.