Page 2274 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 2274
Chapter 135 Hemophilia A and B 2021
TABLE Plasma-derived Recombinant Recombinant FVIII +
135.11 Challenges to Successful Hemophilia Gene Therapy FVIII FVIII Recombinant VWF
1. Efficient transgene delivery
2. Persistent therapeutic transgene expression
3. Host immunologic responses
a. To the transgene product: inhibitors Severe hemophilia A therapy
b. To the vector 2017-2022
• Antivector antibodies
• Antivector cytotoxic T-cell response
FVIII Novel Modified FVIII
conjugates intrinsic (e.g., fusion proteins)
vector infusion, there were no adverse events, but none of those (e.g., PEG) tenase
approaches increased FVIII or FIX levels beyond a few days, and even
then, levels were in the 1% to 4% range.
In contrast, the AAV trials of gene transfer have shown evidence FVIII Novel adjunctive
of therapeutic efficacy. There have now been three completed AAV gene therapies
FIX trials, the first into skeletal muscle and the latter two into liver. transfer (i.e., antifibrinolysis,
Both of the liver-directed trials, the first using hepatic artery delivery TFPI/PC inhibition)
of AAV-2 and the second systemic intravenous delivery of AAV-8,
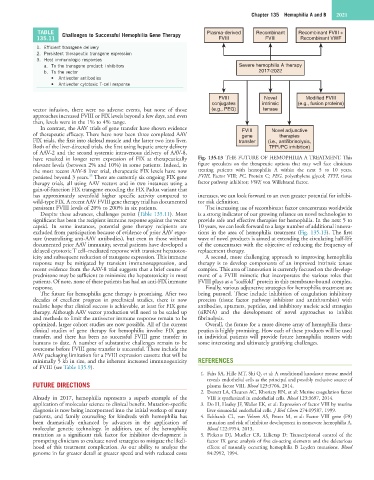
have resulted in longer term expression of FIX at therapeutically Fig. 135.13 THE FUTURE OF HEMOPHILIA A TREATMENT. This
relevant levels (between 2% and 10%) in some patients. Indeed, in figure speculates on the therapeutic options that may well face clinicians
the most recent AAV-8 liver trial, therapeutic FIX levels have now treating patients with hemophilia A within the next 5 to 10 years.
35
persisted beyond 3 years. There are currently six ongoing FIX gene FVIII, Factor VIII; PC, Protein C; PEG, polyethylene glycol; TFPI, tissue
therapy trials, all using AAV vectors and in two instances using a factor pathway inhibitor; VWF, von Willebrand factor.
gain-of-function FIX transgene encoding the FIX Padua variant that
has approximately sevenfold higher specific activity compared to increases, we can look forward to an even greater potential for inhibi-
wild-type FIX. A recent AAV FVIII gene therapy trial has documented tor risk definition.
persistent FVIII levels of 20% to 200% in six patients. The increasing use of recombinant factor concentrates worldwide
Despite these advances, challenges persist (Table 135.11). Most is a strong indicator of our growing reliance on novel technologies to
significant has been the recipient immune response against the vector provide safe and effective therapies for hemophilia. In the next 5 to
capsid. In some instances, potential gene therapy recipients are 10 years, we can look forward to a large number of additional innova-
excluded from participation because of evidence of prior AAV expo- tions in the area of hemophilia treatment (Fig. 135.13). The first
sure (neutralizing anti-AAV antibodies), but even in those without wave of novel products is aimed at extending the circulating half-life
documented prior AAV immunity, several patients have developed a of the concentrates with the objective of reducing the frequency of
delayed cytotoxic T cell–mediated response with transient hepatotox- replacement therapy.
icity and subsequent reduction of transgene expression. This immune A second, more challenging approach to improving hemophilia
response may be mitigated by transient immunosuppression, and therapy is to develop components of an improved intrinsic tenase
recent evidence from the AAV-8 trial suggests that a brief course of complex. This area of innovation is currently focused on the develop-
prednisone may be sufficient to minimize the hepatotoxicity in most ment of a FVIII mimetic that incorporates the various roles that
patients. Of note, none of these patients has had an anti-FIX immune FVIII plays as a “scaffold” protein in this membrane-bound complex.
response. Finally, various adjunctive strategies for hemophilia treatment are
The future for hemophilia gene therapy is promising. After two being pursued. These include inhibition of coagulation inhibitory
decades of excellent progress in preclinical studies, there is now proteins (tissue factor pathway inhibitor and antithrombin) with
realistic hope that clinical success is achievable, at least for FIX gene antibodies, aptamers, peptides, and inhibitory nucleic acid strategies
therapy. Although AAV vector production will need to be scaled up (siRNA) and the development of novel approaches to inhibit
and methods to limit the antivector immune response remain to be fibrinolysis.
optimized, larger cohort studies are now possible. All of the current Overall, the future for a more diverse array of hemophilia thera-
clinical studies of gene therapy for hemophilia involve FIX gene peutics is highly promising. How each of these products will be used
transfer, and there has been no successful FVIII gene transfer in in individual patients will provide future hemophilia treaters with
humans to date. A number of substantive challenges remain to be some interesting and ultimately gratifying challenges.
overcome before FVIII gene transfer is successful. These include the
AAV packaging limitation for a FVIII expression cassette that will be
minimally 5 kb in size, and the inherent increased immunogenicity REFERENCES
of FVIII (see Table 135.9).
1. Fahs SA, Hille MT, Shi Q, et al: A conditional knockout mouse model
reveals endothelial cells as the principal and possibly exclusive source of
FUTURE DIRECTIONS plasma factor VIII. Blood 123:3706, 2014.
2. Everett LA, Cleuren AC, Khoriaty RN, et al: Murine coagulation factor
Already in 2017, hemophilia represents a superb example of the VIII is synthesized in endothelial cells. Blood 123:3697, 2014.
application of molecular science to clinical benefit. Mutation-specific 3. Do H, Healey JF, Waller EK, et al: Expression of factor VIII by murine
diagnosis is now being incorporated into the initial workup of many liver sinusoidal endothelial cells. J Biol Chem 274:19587, 1999.
patients, and family counseling for kindreds with hemophilia has 4. Eckhardt CL, van Velzen AS, Peters M, et al: Factor VIII gene (F8)
been dramatically enhanced by advances in the application of mutation and risk of inhibitor development in nonsevere hemophilia A.
molecular genetic technology. In addition, use of the hemophilic Blood 122:1954, 2013.
mutation as a significant risk factor for inhibitor development is 5. Picketts DJ, Mueller CR, Lillicrap D: Transcriptional control of the
prompting clinicians to evaluate novel strategies to mitigate the likeli- factor IX gene: analysis of five cis-acting elements and the deleterious
hood of this treatment complication. As our ability to analyze the effects of naturally occurring hemophilia B Leyden mutations. Blood
genome in far greater detail at greater speed and with reduced costs 84:2992, 1994.