Page 1713 - Williams Hematology ( PDFDrive )
P. 1713
1688 Part XI: Malignant Lymphoid Diseases Chapter 103: Cutaneous T-Cell Lymphoma (Mycosis Fungoides and Sézary Syndrome) 1689
14
infections, leading to death in the majority of patients who develop this with a worse prognosis. In some cases, distinction between LyP and
144
complication. Combination therapy produces objective responses in PCALCL cannot be made because of discrepancies between clinical fea-
greater than 80 percent of patients and complete responses in approx- tures and histologic appearance. These cases are referred to as borderline
imately one fourth of cases. 99,145 The duration of remission varies, with lesions, and their classification should take into consideration their clin-
a median of approximately 1 year. No long-term disease-free survival ical behavior and appearance (Fig. 103–7A).
has been reported. Other CD30+ cutaneous lymphoproliferative disorders include
Combined Modality Therapy Several multidrug regimens large cell transformation of MF, systemic anaplastic large cell lymphoma
reportedly improve clinical response in patients with MF, including (ALCL), cutaneous NK/T-cell lymphoma, and Hodgkin lymphoma.
combination of extracorporeal photophoresis with low-dose interferon-α Making the distinctions between these diagnoses is critical because
and oral bexarotene; prednisone and fludarabine; and PUVA and oral management and prognosis are significantly different (see “Treatment”
bexarotene. 3,146 below). The descriptive term anaplastic could be omitted from the name
Because in general MF is an indolent malignancy of T cells with of this lymphoma because these lymphomas may have an anaplastic,
excellent prognosis in early stages, the treatment should be conser- immunoblastic, or pleomorphic cell morphology. Regardless of patho-
vative, with skin-directed therapies (nitrogen mustard, topical gluco- logic type, these CD30+ large cell lymphomas have a similar clinical
corticoids, topical bexarotene) combined with light therapy, low-dose course, treatment, and prognosis. 81,147–149
interferon, low-dose methotrexate, or other single-agent chemotherapy. CD30+ PCALCL can occur at any age, with the peak incidence in
The survival of patients treated with aggressive chemotherapy is not dif- patients in their 60s, with a slight male predominance. 79,150 PCALCL can
ferent from the survival of patients treated conservatively, but aggressive occur anywhere on the body. The lesions are brownish to violaceous
chemotherapy results in greater toxicity. Because no curative therapy nodules or tumors, ranging in number from solitary (most commonly)
exists, the goal of therapy is to prevent progression to more advanced to numerous with generalized involvement. They may regress sponta-
stages and to preserve the patient’s quality of life for as long as possible. neously. Histopathologically, at least 75 percent of the large cells should
express CD30. Most cases are CD4+, with loss of pan–T-cell markers
PROGNOSIS CD2, CD3, and CD5. In rare cases, the cells are CD8+CD30+. In con-
trast to systemic ALCL, primary cutaneous large cell lymphoma is neg-
151
Prognosis largely depends on the stage at presentation. Fifty percent of ative for CD15 and epithelial membrane antigen. In addition, primary
deaths among patients with MF result from infections. Septicemia and cutaneous large cell lymphoma usually does not express anaplastic lym-
bacterial pneumonia are common; they usually are caused by Staphylo- phoma kinase-1 (ALK-1) or the t(2;5) chromosomal translocation. 152,153
coccus or Pseudomonas and develop from cutaneous lesions. Herpes Presence of ALK-1 in cutaneous lesions without systemic involvement
54
virus infections occur in up to 10 percent of patients with advanced MF. does not carry a worse prognosis.
Progressive MF with widespread visceral involvement late in the course
of the disease is the next most common cause of death.
LYMPHOMATOID PAPULOSIS
PRIMARY CUTANEOUS ANAPLASTIC LyP is the benign counterpart of primary cutaneous ALCL. It is charac-
LARGE CELL LYMPHOMA terized by crops of erythematous, dome-shaped papules or nodules that
may ulcerate spontaneously. It regresses over a few months with minor
CLINICAL FINDINGS sequelae such as scarring or atrophy (see Fig. 103–7B). The three main
histologic types of LyP are A, B, and C. The infiltrate usually is wedge
CD30+ cutaneous lymphoproliferative disorders are the second most shaped with ulcer formation. The large atypical cells of type A resemble
common CTCLs after MF and represent approximately 25 percent of immunoblasts of Reed-Sternberg cells. These cells are surrounded by
CTCL cases. PCALCL represents a spectrum of CD30+ lymphoprolif- neutrophils and eosinophils. Type B cells resemble MF, with lichenoid
81
erative disorders, including LyP and PCALCL as its malignant counter- lymphocytic infiltration of cells with cerebriform nuclei and some epi-
part. It is defined by the presence of skin involvement without evidence dermotropism. Type C cells resemble ALCL, with sheets of large CD30+
of extracutaneous disease for at least 6 months after presentation. Sec- cells in the infiltrate. The histologic distinction between LyP and the
13
ondary involvement of lymph nodes may not necessarily be associated corresponding condition may be difficult, and clinical correlation is
A B
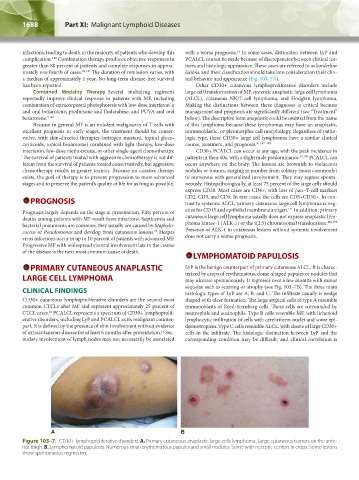
Figure 103–7. CD30+ lymphoproliferative disorders. A. Primary cutaneous anaplastic large cells lymphoma. Large cutaneous tumors on the ante-
rior thigh. B. Lymphomatoid papulosis. Numerous small erythematous papules and small nodules. Some with necrotic centers in crops. Some lesions
show spontaneous regression.
Kaushansky_chapter 103_p1679-1692.indd 1688 9/21/15 12:51 PM