Page 890 - Williams Hematology ( PDFDrive )
P. 890
864 Part VI: The Erythrocyte Chapter 56: Hypersplenism and Hyposplenism 865
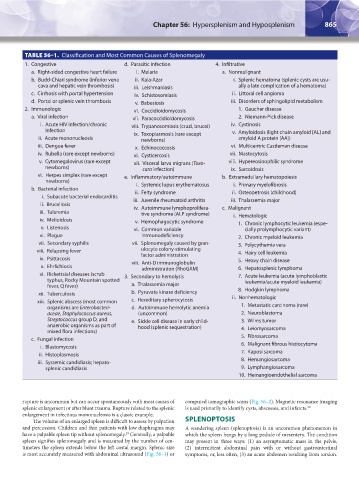
TABLE 56–1. Classification and Most Common Causes of Splenomegaly
1. Congestive d. Parasitic infection 4. Infiltrative
a. Right-sided congestive heart failure i. Malaria a. Nonmalignant
b. Budd-Chiari syndrome (inferior vena ii. Kala-Azar i. Splenic hematoma (splenic cysts are usu-
cava and hepatic vein thrombosis) iii. Leishmaniasis ally a late complication of a hematoma)
c. Cirrhosis with portal hypertension iv. Schistosomiasis ii. Littoral cell angioma
d. Portal or splenic vein thrombosis v. Babesiosis iii. Disorders of sphingolipid metabolism
2. Immunologic vi. Coccidioidomycosis 1. Gaucher disease
a. Viral infection vii. Paracoccidioidomycosis 2. Niemann-Pick disease
i. Acute HIV infection/chronic viii. Trypanosomiasis (cruzi, brucei) iv. Cystinosis
Infection ix. Toxoplasmosis (rare except v. Amyloidosis (light chain amyloid [AL] and
ii. Acute mononucleosis newborns) amyloid A protein [AA])
iii. Dengue fever x. Echinococcosis vi. Multicentric Castleman disease
iv. Rubella (rare except newborns) xi. Cysticercosis vii. Mastocytosis
v. Cytomegalovirus (rare except xii. Visceral larva migrans (Toxo- viii. Hypereosinophilic syndrome
newborns) cara infection) ix. Sarcoidosis
vi. Herpes simplex (rare except e. Inflammatory/autoimmune b. Extramedullary hematopoiesis
newborns) i. Systemic lupus erythematosus i. Primary myelofibrosis
b. Bacterial infection ii. Felty syndrome ii. Osteopetrosis (childhood)
i. Subacute bacterial endocarditis iii. Juvenile rheumatoid arthritis iii. Thalassemia major
ii. Brucellosis iv. Autoimmune lymphoprolifera- c. Malignant
iii. Tularemia tive syndrome (ALP syndrome) i. Hematologic
iv. Melioidosis v. Hemophagocytic syndrome 1. Chronic lymphocytic leukemia (espe-
v. Listeriosis vi. Common variable cially prolymphocytic variant)
vi. Plague immunodeficiency 2. Chronic myeloid leukemia
vii. Secondary syphilis vii. Splenomegaly caused by gran- 3. Polycythemia vera
viii. Relapsing fever ulocyte colony-stimulating 4. Hairy cell leukemia
ix. Psittacosis factor administration 5. Heavy chain disease
x. Ehrlichiosis viii. Anti-D immunoglobulin 6. Hepatosplenic lymphoma
administration (RhoGAM)
xi. Rickettsial diseases (scrub 3. Secondary to hemolysis 7. Acute leukemia (acute lymphoblastic
typhus, Rocky Mountain spotted leukemia/acute myeloid leukemia)
fever, Q fever) a. Thalassemia major 8. Hodgkin lymphoma
xii. Tuberculosis b. Pyruvate kinase deficiency ii. Nonhematologic
xiii. Splenic abscess (most common c. Hereditary spherocytosis
organisms are Enterobacteri- d. Autoimmune hemolytic anemia 1. Metastatic carcinoma (rare)
aceae, Staphylococcus aureus, (uncommon) 2. Neuroblastoma
Streptococcus group D, and e. Sickle cell disease in early child- 3. Wilms tumor
anaerobic organisms as part of hood (splenic sequestration) 4. Leiomyosarcoma
mixed flora infections)
c. Fungal infection 5. Fibrosarcoma
i. Blastomycosis 6. Malignant fibrous histiocytoma
ii. Histoplasmosis 7. Kaposi sarcoma
iii. Systemic candidiasis; hepato- 8. Hemangiosarcoma
splenic candidiasis 9. Lymphangiosarcoma
10. Hemangioendothelial sarcoma
rupture is uncommon but can occur spontaneously with most causes of computed tomographic scans (Fig. 56–2). Magnetic resonance imaging
splenic enlargement or after blunt trauma. Rupture related to the splenic is used primarily to identify cysts, abscesses, and infarcts. 30
enlargement in infectious mononucleosis is a classic example.
The volume of an enlarged spleen is difficult to assess by palpation SPLENOPTOSIS
and percussion. Children and thin patients with low diaphragms may A wandering spleen (splenoptosis) is an uncommon phenomenon in
have a palpable spleen tip without splenomegaly. Generally, a palpable which the spleen hangs by a long pedicle of mesentery. The condition
29
spleen signifies splenomegaly and is measured by the number of cen- may present in three ways: (1) an asymptomatic mass in the pelvis,
timeters the spleen extends below the left costal margin. Splenic size (2) intermittent abdominal pain with or without gastrointestinal
is most accurately measured with abdominal ultrasound (Fig. 56–1) or symptoms, or, less often, (3) an acute abdomen resulting from torsion.
Kaushansky_chapter 56_p0863-0870.indd 865 9/17/15 3:05 PM