Page 1191 - Clinical Immunology_ Principles and Practice ( PDFDrive )
P. 1191
1156 ParT TEN Prevention and Therapy of Immunological Diseases
34
34 34
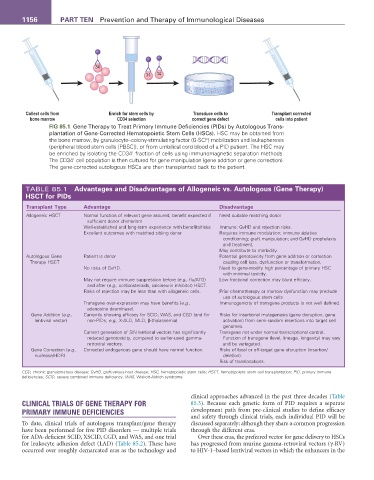
Collect cells from Enrich for stem cells by Transduce cells to Transplant corrected
bone marrow CD34 selection correct gene defect cells into patient
FIG 85.1 Gene Therapy to Treat Primary Immune Deficiencies (PIDs) by Autologous Trans-
plantation of Gene-Corrected Hematopoietic Stem Cells (HSCs). HSC may be obtained from
the bone marrow, by granulocyte–colony-stimulating factor (G-SCF) mobilization and leukapheresis
(peripheral blood stem cells [PBSC]), or from umbilical cord blood of a PID patient. The HSC may
+
be enriched by isolating the CD34 fraction of cells using immunomagnetic separation methods.
+
The CD34 cell population is then cultured for gene manipulation (gene addition or gene correction).
The gene-corrected autologous HSCs are then transplanted back to the patient.
TABLE 85.1 advantages and Disadvantages of allogeneic vs. autologous (Gene Therapy)
HSCT for PIDs
Transplant Type advantage Disadvantage
Allogeneic HSCT Normal function of relevant gene assured; benefit expected if Need suitable matching donor
sufficient donor chimerism
Well-established and long-term experience with benefits/risks Immune: GvHD and rejection risks.
Excellent outcomes with matched sibling donor Requires immune modulation: immune ablative
conditioning; graft manipulation; and GvHD prophylaxis
and treatment.
May contribute to morbidity.
Autologous Gene Patient is donor Potential genotoxicity from gene addition or correction
Therapy HSCT causing cell loss, dysfunction or transformation.
No risks of GvHD. Need to gene-modify high percentage of primary HSC
with minimal toxicity.
May not require immune suppression before (e.g., flu/ATG) Low fractional correction may blunt efficacy.
and after (e.g., corticosteroids, calcineurin inhibitor) HSCT.
Risks of rejection may be less than with allogeneic cells. Prior chemotherapy or marrow dysfunction may preclude
use of autologous stem cells
Transgene over-expression may have benefits (e.g., Immunogenicity of transgene products is not well defined.
adenosine deaminase).
Gene Addition (e.g., Currently showing efficacy for SCID, WAS, and CGD (and for Risks for insertional mutagenesis (gene disruption, gene
lentiviral vector) non-PIDs; e.g., X-ALD, MLD, β-thalassemia). activation) from semi-random insertions into target cell
genomes.
Current generation of SIN lentiviral vectors has significantly Transgene not under normal transcriptional control.
reduced genotoxicity, compared to earlier-used gamma- Function of transgene (level, lineage, longevity) may vary
retroviral vectors. and be variegated.
Gene Correction (e.g., Corrected endogenous gene should have normal function. Risks of local or off-target gene disruption (insertion/
nuclease/HDR) deletion).
Risk of translocations.
CGD, chronic granulomatous disease; GvHD, graft-versus-host disease; HSC, hematopoietic stem cells; HSCT, hematopoietic stem cell transplantation; PID, primary immune
deficiencies; SCID, severe combined immune deficiency; WAS, Wiskott-Aldrich syndrome.
clinical approaches advanced in the past three decades (Table
CLINICAL TRIALS OF GENE THERAPY FOR 85.3). Because each genetic form of PID requires a separate
PRIMARY IMMUNE DEFICIENCIES development path from pre-clinical studies to define efficacy
and safety through clinical trials, each individual PID will be
To date, clinical trials of autologous transplant/gene therapy discussed separately; although they share a common progression
have been performed for five PID disorders — multiple trials through the different eras.
for ADA-deficient SCID, XSCID, CGD, and WAS, and one trial Over these eras, the preferred vector for gene delivery to HSCs
for leukocyte adhesion defect (LAD) (Table 85.2). These have has progressed from murine gamma-retroviral vectors (γ-RV)
occurred over roughly demarcated eras as the technology and to HIV-1–based lentiviral vectors in which the enhancers in the