Page 1460 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 1460
CHAPTER 104: Jaundice, Diarrhea, Obstruction, and Pseudoobstruction 999
■ ETIOLOGY OF JAUNDICE Jaundice
Table 104-1 lists possible causes of jaundice. The key step to determine
management relies on differentiating whether the cause of hyperbiliru-
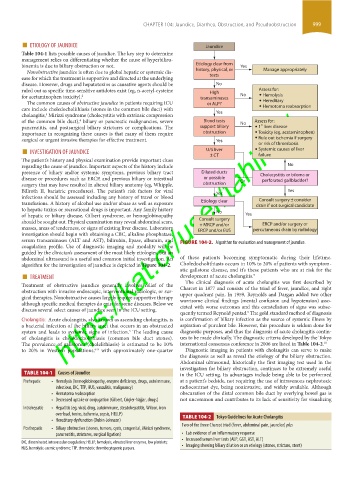
binemia is due to biliary obstruction or not. Etiology clear from Yes
Nonobstructive jaundice is often due to global hepatic or systemic dis- history, physical, or Manage appropriately
ease for which the treatment is supportive and directed at the underlying tests
disease. However, drugs and hepatotoxins as causative agents should be No
ruled out as specific time-sensitive antidotes exist (eg, n-acetyl-cysteine High Assess for:
for acetaminophen toxicity). 2 transaminases No Hemolysis
The common causes of obstructive jaundice in patients requiring ICU or ALP? Hereditary
https://kat.cr/user/tahir99/
care include choledocholithiasis (stones in the common bile duct) with Hemotoma reabsorption
3
cholangitis, Mirizzi syndrome (cholecystitis with extrinsic compression Yes
of the common bile duct), biliary or pancreatic malignancies, severe Blood tests No Assess for:
4
º
pancreatitis, and postsurgical biliary strictures or complications. The support biliary 1 liver disease
importance in recognizing these causes is that many of them require obstruction Toxicity (eg, acetaminophen)
surgical or urgent invasive therapies for effective treatment. Yes Rule out ischemia if surgery
■ INVESTIGATION OF JAUNDICE U/S liver Systemic causes of liver
or risk of thrombosis
The patient’s history and physical examination provide important clues ± CT failure
regarding the cause of jaundice. Important aspects of the history include No
presence of biliary and/or systemic symptoms, previous biliary tract Dilated ducts Cholecystitis or biloma or
disease or procedures such as ERCP, and previous biliary or intestinal or possible Or perforated gallbladder?
surgery that may have resulted in altered biliary anatomy (eg, Whipple, obstruction
Billroth II, bariatric procedures). The patient’s risk factors for viral Yes Yes
infections should be assessed including any history of travel or blood
Consult surgery ± consider
transfusions. A history of alcohol use and/or abuse as well as exposure Etiology clear drain if not surgical candidate
to hepatic toxins or recreational drugs is important. Any family history
of hepatic or biliary disease, Gilbert syndrome, or hemoglobinopathy No Yes
should be sought out. Physical examination may reveal abdominal scars, Consult surgery ERCP and/or surgery or
+ MRCP and/or
masses, areas of tenderness, or signs of existing liver disease. Laboratory ERCP and/or EUS percutaneous drain by radiology
investigation should begin with obtaining a CBC, alkaline phosphatase,
serum transaminases (ALT and AST), bilirubin, lipase, albumin, and FIGURE 104-2. Algorithm for evaluation and management of jaundice.
coagulation profile. Use of diagnostic imaging and modality will be
guided by the clinician’s assessment of the most likely etiologies, but an
abdominal ultrasound is a useful and common initial investigation. An of these patients becoming symptomatic during their lifetime.
algorithm for the investigation of jaundice is depicted in Figure 104-2. Choledocholithiasis occurs in 10% to 20% of patients with symptom-
■ TREATMENT atic gallstone disease, and it’s these patients who are at risk for the
development of acute cholangitis.
5
The clinical diagnosis of acute cholangitis was first described by
Treatment of obstructive jaundice generally involves relief of the Charcot in 1877 and consists of the triad of fever, jaundice, and right
obstruction with invasive endoscopic, interventional radiologic, or sur- upper quadrant pain. In 1959, Reynolds and Dargan added two other
gical therapies. Nonobstructive causes largely require supportive therapy worrisome clinical findings (mental confusion and hypotension) asso-
although specific medical therapies do exist for some diseases. Below we ciated with worse outcomes and this constellation of signs was subse-
discuss several select causes of jaundice seen in the ICU setting.
quently termed Reynold pentad. The gold standard method of diagnosis
9
Cholangitis: Acute cholangitis, also known as ascending cholangitis, is is confirmation of biliary infection as the source of systemic illness by
a bacterial infection of the biliary tract that occurs in an obstructed aspiration of purulent bile. However, this procedure is seldom done for
5
system and leads to systemic signs of infection. The leading cause diagnostic purposes, and thus the diagnosis of acute cholangitis contin-
of cholangitis is choledocholithiasis (common bile duct stones). ues to be made clinically. The diagnostic criteria developed by the Tokyo
The prevalence of gallstones (cholelithiasis) is estimated to be 10% international consensus conference in 2006 are listed in Table 104-2. 10
to 20% in Western populations, with approximately one-quarter Diagnostic imaging in patients with cholangitis can serve to make
6-8
the diagnosis as well as reveal the etiology of the biliary obstruction.
Abdominal ultrasound, historically the first imaging test used in the
investigation for biliary obstruction, continues to be extremely useful
TABLE 104-1 Causes of Jaundice in the ICU setting. Its advantages include being able to be performed
Prehepatic • Hemolysis (hemoglobinopathy, enzyme deficiency, drugs, autoimmune, at a patient’s bedside, not requiring the use of intravenous nephrotoxic
infectious, DIC, TTP, HUS, vasculitis, malignancy) radiocontrast dye, being noninvasive, and widely available. Although
• Hematoma reabsorption obscuration of the distal common bile duct by overlying bowel gas is
• Decreased uptake or conjugation (Gilbert, Crigler-Najjar, drugs) not uncommon and contributes to its lack of sensitivity for visualizing
Intrahepatic • Hepatitis (eg, viral, drug, autoimmune, steatohepatitis, Wilson, iron
overload, toxins, ischemia, sepsis, HELLP) TABLE 104-2 Tokyo Guidelines for Acute Cholangitis
• Hereditary dysfunction (Dubin-Johnson)
Two of the three Charcot triad (fever, abdominal pain, jaundice) plus
Posthepatic • Biliary obstruction (stones, tumors, cysts, congenital, Mirizzi syndrome,
pancreatitis, strictures, surgical ligation) • Lab evidence of an inflammatory response
• Increased serum liver tests (ALP, GGT, AST, ALT)
DIC, disseminated intravascular coagulation; HELLP, hemolysis, elevated liver enzymes, low platelets; • Imaging showing biliary dilation or an etiology (stones, stricture, stent)
HUS, hemolytic-uremic syndrome; TTP, thrombotic thrombocytopenic purpura.
section09.indd 999 1/14/2015 9:27:04 AM