Page 1476 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 1476
CHAPTER 105: Gastrointestinal Hemorrhage 1015
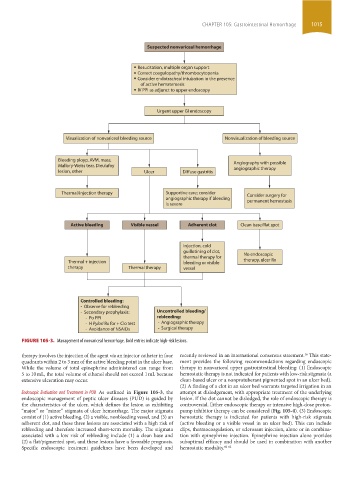
Suspected nonvariceal hemorrhage
Resucitation, multiple organ support
Correct coagulopathy/thrombocytopenia
Consider endotracheal intubation in the presence
of active hematemesis
IV PPI as adjunct to upper endoscopy
Urgent upper GI endoscopy
Visualization of nonvariceal bleeding source Nonvisualization of bleeding source
Bleeding ployp, AVM, mass, Angiography with possible
Mallory-Weiss tear, Dieulafoy angiographic therapy
lesion, other Ulcer Diffuse gastritis
Thermal/injection therapy Supportive care; consider Consider surgery for
angiographic therapy if bleeding permanent hemostasis
is severe
Active bleeding Visible vessel Adherent clot Clean base/flat spot
Injection, cold
guillotining of clot, No endoscopic
thermal therapy for
Thermal + injection bleeding or visible therapy, ulcer Rx
therapy Thermal therapy vessel
Controlled bleeding:
- Observe for rebleeding
- Secondary prophylaxis: Uncontrolled bleeding/
- Po PPI rebleeding:
- H Pylori Rx for + Clo test - Angiographic therapy
- Avoidance of NSAIDs - Surgical therapy
FIGURE 105-3. Management of nonvariceal hemorrhage. Bold entries indicate high-risk lesions.
16
therapy involves the injection of the agent via an injector catheter in four recently reviewed in an international consensus statement. This state-
quadrants within 2 to 3 mm of the active bleeding point in the ulcer base. ment provides the following recommendations regarding endoscopic
While the volume of total epinephrine administered can range from therapy in nonvariceal upper gastrointestinal bleeding: (1) Endoscopic
5 to 10 mL, the total volume of ethanol should not exceed 1 mL because hemostatic therapy is not indicated for patients with low-risk stigmata (a
extensive ulceration may occur. clean-based ulcer or a nonprotuberant pigmented spot in an ulcer bed).
(2) A finding of a clot in an ulcer bed warrants targeted irrigation in an
Endoscopic Evaluation and Treatment in PUD As outlined in Figure 105-3, the attempt at dislodgement, with appropriate treatment of the underlying
endoscopic management of peptic ulcer diseases (PUD) is guided by lesion. If the clot cannot be dislodged, the role of endoscopic therapy is
the characteristics of the ulcer, which defines the lesion as exhibiting controversial. Either endoscopic therapy or intensive high-dose proton-
“major” or “minor” stigmata of ulcer hemorrhage. The major stigmata pump inhibitor therapy can be considered (Fig. 105-4). (3) Endoscopic
consist of (1) active bleeding, (2) a visible, nonbleeding vessel, and (3) an hemostatic therapy is indicated for patients with high-risk stigmata
adherent clot, and these three lesions are associated with a high risk of (active bleeding or a visible vessel in an ulcer bed). This can include
rebleeding and therefore increased short-term mortality. The stigmata clips, thermocoagulation, or sclerosant injection, alone or in combina-
associated with a low risk of rebleeding include (1) a clean base and tion with epinephrine injection. Epinephrine injection alone provides
(2) a flat/pigmented spot, and these lesions have a favorable prognosis. suboptimal efficacy and should be used in combination with another
Specific endoscopic treatment guidelines have been developed and hemostatic modality. 60-62
section09.indd 1015 1/14/2015 9:27:12 AM