Page 1528 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 1528
CHAPTER 110: Special Considerations in the Surgical Patient 1047
nutritional support before and immediately after surgery. Early insti-
17
tution of enteric feeding has been shown to be of benefit, including
a reduction in septic sequelae, in surgical patients undergoing intra-
abdominal procedures. If daily caloric intake goal could not be
18
achieved with enteral feeding alone before day 8 of ICU admission, insti- hemorrhage
tution of parenteral nutritional support should be considered to prevent Hypertension
Compensated
further loss of muscle mass. Earlier initiation of parenteral nutrition Hemorrhagic
19
appears to be associated with more infectious complications, delayed shock
recovery, and higher health care costs. Adequate nutrition affects not
19
only the maintenance of muscle mass, but also the maintenance of respi- Increasing vascular tone
ratory function, and thus both dependence on ventilatory support and
weaning from mechanical ventilatory assistance. Anesthesia
■ MAGNITUDE AND DURATION OF SURGICAL INSULT
Since the duration and magnitude of surgical procedures affect the Hypotension
intensity of the metabolic and endocrine response, the aim should be to Septic
decrease the magnitude, duration, and frequency of surgical insults shock
to the critically ill patient, particularly patients with poor nutritional and
cardiorespiratory reserve. This goal, however, must be considered in the
context of the underlying problem. The magnitude and duration of Increasing blood volume
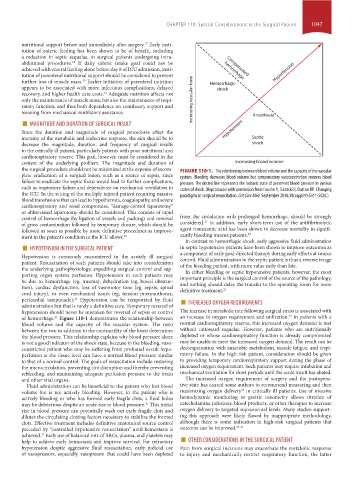
the surgical procedure should not be minimized at the expense of incom- FIGURE 110-1. The relationship between blood volume and the capacity of the vascular
plete eradication of a surgical lesion, such as a source of sepsis, since system. Bleeding decreases blood volume but compensatory vasoconstriction restores blood
failure to eradicate the septic focus would lead to further complications, pressure. The dotted line represents the isobaric state of preserved blood pressure in various
such as respiratory failure and dependence on mechanical ventilation in states of shock. (Reproduced with permission from Fouche Y, Sikorski R, Dutton RP. Changing
the ICU. In the setting of the multiply injured patient requiring massive paradigms in surgical resuscitation. Crit Care Med. September 2010;38(suppl 9):S411-S420.)
blood transfusions that can lead to hypothermia, coagulopathy, and severe
cardiorespiratory and renal compromise, “damage-control laparotomy”
or abbreviated laparotomy should be considered. This consists of rapid
control of hemorrhage (by ligation of vessels and packing) and removal from the circulation with prolonged hemorrhage, should be strongly
21
of gross contamination followed by temporary closure, which should be considered. In addition, early short-term use of the antifibrinolytic
followed as soon as possible by more definitive procedures as improve- agent tranexamic acid has been shown to decrease mortality in signifi-
ment in the patient’s condition in the ICU allows. 20 cantly bleeding trauma patients. 22
■ HYPOTENSION IN THE SURGICAL PATIENT in septic hypotensive patients have been shown to improve outcomes as
In contrast to hemorrhagic shock, early aggressive fluid administration
Hypotension is commonly encountered in the acutely ill surgical a component of early goal-directed therapy during early efforts at source
patient. Resuscitation of such patients should take into consideration control. Fluid administration in the septic patient is thus a reverse image
of the bleeding patient, with more value early than late.
the underlying pathophysiology, expediting surgical control and sup-
In either bleeding or septic hypotensive patients, however, the most
porting organ system perfusion. Hypotension in such patients may important principle is the surgical control of the source of the pathology,
be due to hemorrhage (eg, trauma), dehydration (eg, bowel obstruc-
tion), cardiac dysfunction, loss of vasomotor tone (eg, sepsis, spinal and nothing should delay the transfer to the operating room for more
definitive treatment.
21
cord injury), or even mechanical issues (eg, tension pneumothorax,
pericardial tamponade). Hypotension can be temporized by fluid ■ INCREASED OXYGEN REQUIREMENTS
21
administration but that is rarely a definitive cure. Temporary reversal of
hypotension should never be mistaken for reversal of sepsis or control The increase in metabolic rate following surgical stress is associated with
23
of hemorrhage. Figure 110-1 demonstrates the relationship between an increase in oxygen requirement and utilization. In patients with a
21
blood volume and the capacity of the vascular system. The ratio normal cardiorespiratory reserve, this increased oxygen demand is met
between the two in addition to the contractility of the heart determines without untoward sequelae. However, patients who are nutritionally
the blood pressure. This relationship explains why blood pressure alone depleted or whose cardiorespiratory function is already compromised
is not a good indicator of the shock state, because in the bleeding, vaso- may be unable to meet the increased oxygen demand. The result can be
constricted patient who may be suffering from profound occult hypo- decompensation with anaerobic metabolism, muscle fatigue, and respi-
perfusion at the tissue level can have a normal blood pressure similar ratory failure. In the high-risk patient, consideration should be given
to that of a normal control. The goals of resuscitation include restoring to providing temporary cardiorespiratory support during the phase of
the microcirculation, preventing clot disruption and thereby preventing increased oxygen requirement. Such patients may require intubation and
rebleeding, and maintaining adequate perfusion pressure to the brain mechanical ventilation for short periods until the acute insult has abated.
and other vital organs. The increased oxygen requirement of surgery and the postopera-
Fluid administration can be beneficial to the patient who lost blood tive state has caused some authors to recommend measuring and then
22
volume but is not actively bleeding. However, in the patient who is maximizing oxygen delivery in critically ill patients. Use of invasive
actively bleeding or who has formed early fragile clots, a fluid bolus hemodynamic monitoring or gastric tonometry allows titration of
may be deleterious despite an acute rise in blood pressure. This initial catecholamine infusions, blood products, or other therapies to increase
21
rise in blood pressure can potentially wash out early fragile clots and oxygen delivery to targeted supranormal levels. Many studies support-
dilutes the circulating clotting factors necessary to stabilize the formed ing this approach were likely flawed by inappropriate methodology,
clots. Effective treatment includes definitive anatomical source control although there is some indication in high-risk surgical patients that
preceded by “controlled hypotensive resuscitation” until hemostasis is outcome can be improved. 23-25
help to achieve early hemostasis and improve survival. For refractory ■ OTHER CONSIDERATIONS IN THE SURGICAL PATIENT
achieved. Early use of balanced mix of RBCs, plasma, and platelets may
21
hypotension despite aggressive fluid resuscitation, early judicial use Pain from surgical incisions may exacerbate the metabolic response
of vasopressors, especially vasopressin that could have been depleted to injury and mechanically restrict respiratory function, the latter
section10.indd 1047 1/20/2015 9:19:29 AM