Page 1636 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 1636
CHAPTER 120: Torso Trauma 1155
paradoxus accurately. The physician should note the difference between
systolic blood pressure during inspiration and expiration. The pressure
waveform will exhibit a lower peak level in inspiration, with higher peak
levels in expiration. The difference between the two peaks is the mea-
sure of the degree of pulsus paradoxus. The degree of pulsus paradoxus
may be determined at the bedside by listening for the first set of sounds
with the sphygmomanometer slowly deflating. The first set of sounds
represents the systolic blood pressure on expiration. As the pressure in
the cuff is slowly released, the gaps in systolic blood pressure sounds
between inspiration and expiration disappear, and there is an increased
frequency of sounds heard with the stethoscope. The difference between
https://kat.cr/user/tahir99/
the initial pressure and the pressure when the gaps in sounds have disap-
Opening in peared is the degree of pulsus paradoxus. Since distended neck veins and
chest wall
(but not gauze pad) hypotension are present in both tension pneumothorax and cardiac tam-
ponade, differentiation between these two conditions is important but at
times difficult. The physician must rely on evidence of hyperresonance
and decreased breath sounds that will suggest tension pneumothorax. If
a search for these signs still leaves doubt, the patient should be treated
Occlusive dressing
(taped on three sides) first for possible tension pneumothorax by insertion of a needle in the
pleural space. This step can be performed quickly and will give the diag-
nosis as well as be therapeutic for a tension pneumothorax. Once tension
Free edge
pneumothorax is ruled out, one should proceed to treatment for cardiac
tamponade if signs of circulatory compromise persist. If immediately
available in the emergency setting, epigastric placement of an ultrasound
probe is also helpful in diagnosing hemopericardium. In many trauma
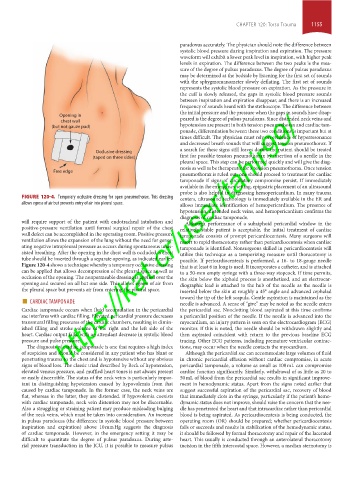
FIGURE 120-4. Temporary occlusive dressing for open pneumothorax. This dressing centers, ultrasound technology is immediately available in the ER and
allows egress of air but prevents entry of air into pleural space. allows immediate identification of hemopericardium. The presence of
hypotension, distended neck veins, and hemopericardium confirms the
diagnosis of cardiac tamponade.
will require support of the patient with endotracheal intubation and Although performance of a subxiphoid pericardial window in the
positive-pressure ventilation until formal surgical repair of the chest relatively stable patient is acceptable, the initial treatment of cardiac
wall defect can be accomplished in the operating room. Positive pressure tamponade consists of prompt pericardiocentesis. Many surgeons will
ventilation allows the expansion of the lung without the need for gener- resort to rapid thoracotomy rather than pericardiocentesis when cardiac
ating negative intrapleural pressure as occurs during spontaneous unas- tamponade is identified. Nonsurgeons skilled in pericardiocentesis will
sisted breathing. After the opening in the chest wall is occluded, a chest utilize this technique as a temporizing measure until thoracotomy is
tube should be inserted through a separate opening, as indicated earlier. possible. If pericardiocentesis is performed, a 16- to 18-gauge needle
Figure 120-4 shows a technique whereby a temporary occlusive dressing that is at least 6 in long is used. It incorporates a catheter, and is attached
can be applied that allows decompression of the pleural space as well as to a 50-mm empty syringe with a three-way stopcock. If time permits,
occlusion of the opening. The nonpermeable dressing is applied over the the skin below the xiphoid process is anesthetized, and an electrocar-
opening and secured on all but one side. This allows egress of air from diographic lead is attached to the hub of the needle as the needle is
the pleural space but prevents air from entering the pleural space. inserted below the skin at roughly a 45° angle and advanced cephalad
■ CARDIAC TAMPONADE toward the tip of the left scapula. Gentle aspiration is maintained as the
needle is advanced. A sense of “give” may be noted as the needle enters
Cardiac tamponade occurs when fluid accumulation in the pericardial the pericardial sac. Nonclotting blood aspirated at this time confirms
sac interferes with cardiac filling. Elevated pericardial pressure decreases a pericardial position of the needle. If the needle is advanced into the
transmural filling pressures of the cardiac chambers, resulting in dimin- myocardium, an injury pattern is seen on the electrocardiogram (ECG)
ished filling and stroke volume of the right and the left side of the monitor. If this is noted, the needle should be withdrawn slightly and
heart. Cardiac output falls, with an attendant decrease in systolic blood then aspirated coincident with return to the previous baseline ECG
pressure and pulse pressure. tracing. Other ECG patterns, including premature ventricular contrac-
The diagnosis of cardiac tamponade is one that requires a high index tions, may occur when the needle contacts the myocardium.
of suspicion and should be considered in any patient who has blunt or Although the pericardial sac can accommodate large volumes of fluid
penetrating trauma to the chest and is hypotensive without any obvious in chronic pericardial effusion without cardiac compromise, in acute
signs of blood loss. The classic triad described by Beck of hypotension, pericardial tamponade, a volume as small as 100 mL can compromise
elevated venous pressure, and muffled heart tones is not always present cardiac function significantly. Similarly, withdrawal of as little as 20 to
or easily discernible. The status of the neck veins is particularly impor- 50 mL of blood from the pericardial sac results in significant improve-
tant in distinguishing hypotension caused by hypovolemia from that ment in hemodynamic status. Apart from the signs noted earlier that
caused by cardiac tamponade. In the former case, the neck veins are suggest successful aspiration of the pericardial sac, recovery of blood
flat, whereas in the latter, they are distended. If hypovolemia coexists that immediately clots in the syringe, particularly if the patient’s hemo-
with cardiac tamponade, neck vein distention may not be discernable. dynamic status does not improve, should raise the concern that the nee-
Also a struggling or straining patient may produce misleading bulging dle has penetrated the heart and that intracardiac rather than pericardial
of the neck veins, which must be taken into consideration. An increase blood is being aspirated. As pericardiocentesis is being conducted, the
in pulsus paradoxus (the difference in systolic blood pressure between operating room (OR) should be prepared; whether pericardiocentesis
inspiration and expiration) above 10 mm Hg suggests the diagnosis fails or succeeds and results in stabilization of the hemodynamic status,
of cardiac tamponade. However, in the emergency setting it may be it should be followed by formal thoracotomy and repair of the lacerated
difficult to quantitate the degree of pulsus paradoxus. During arte- heart. This usually is conducted through an anterolateral thoracotomy
rial pressure transduction in the ICU, it is possible to measure pulsus incision in the fifth intercostal space. However, a median sternotomy is
section10.indd 1155 1/20/2015 9:21:07 AM