Page 1635 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 1635
1154 PART 10: The Surgical Patient
for dealing with thoracic trauma generally are within the scope of most
practicing intensivists. Of the injuries that require open surgical inter- A B C
vention, most do not require the expertise of a trained thoracic surgeon.
From the intensivist’s standpoint, resuscitative measures are aimed at
correcting hypoxemia and maintaining normal hemodynamic status.
These two aims are achieved by techniques for establishing patency of
the airway, chest decompression for evacuating fluid or air, pericardio-
centesis, and vascular access for fluid administration.
In addition to upper airway obstruction, the following thoracic inju-
ries require immediate intervention:
1. Tension pneumothorax
2. Open pneumothorax
3. Cardiac tamponade
4. Massive hemothorax
5. Massive pneumothorax
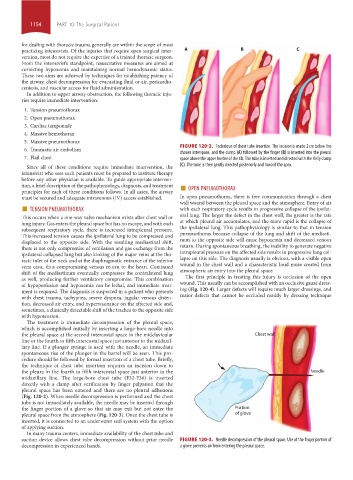
6. Traumatic air embolism FIGURE 120-2. Technique of chest tube insertion. The incision is made 2 cm below the
chosen interspace, and the clamp (A) followed by the finger (B) is inserted into the pleural
7. Flail chest space above the upper border of the rib. The tube is inserted and directed with the Kelly clamp
Since all of these conditions require immediate intervention, the (C). The tube is then gently directed posteriorly and toward the apex.
intensivist who sees such patients must be prepared to institute therapy
before any other physician is available. To guide appropriate interven-
tion, a brief description of the pathophysiology, diagnosis, and treatment ■ OPEN PNEUMOTHORAX
principles for each of these conditions follows. In all cases, the airway
must be secured and adequate intravenous (IV) access established. In open pneumothorax, there is free communication through a chest
■ TENSION PNEUMOTHORAX wall wound between the pleural space and the atmosphere. Entry of air
with each respiratory cycle results in progressive collapse of the ipsilat-
This occurs when a one-way valve mechanism exists after chest wall or eral lung. The larger the defect in the chest wall, the greater is the rate
lung injury. Gas enters the pleural space but has no escape, and with each at which pleural air accumulates, and the more rapid is the collapse of
subsequent respiratory cycle, there is increased intrapleural pressure. the ipsilateral lung. This pathophysiology is similar to that in tension
This increased tension causes the ipsilateral lung to be compressed and pneumothorax because collapse of the lung and shift of the mediasti-
displaced to the opposite side. With the resulting mediastinal shift, num to the opposite side will cause hypoxemia and decreased venous
there is not only compromise of ventilation and gas exchange from the return. During spontaneous breathing, the inability to generate negative
ipsilateral collapsed lung but also kinking of the major veins at the tho- intrapleural pressure on the affected side results in progressive lung col-
racic inlet of the neck and at the diaphragmatic entrance of the inferior lapse on this side. The diagnosis usually is obvious, with a visible open
vena cava, thus compromising venous return to the heart. Continued wound in the chest wall and a characteristic loud noise created from
shift of the mediastinum eventually compresses the contralateral lung atmospheric air entry into the pleural space.
as well, producing further ventilatory compromise. This combination The first principle in treating this injury is occlusion of the open
of hypoperfusion and hypoxemia can be lethal, and immediate treat- wound. This usually can be accomplished with an occlusive gauze dress-
ment is required. The diagnosis is suspected in a patient who presents ing (Fig. 120-4). Larger defects will require much larger dressings, and
with chest trauma, tachypnea, severe dyspnea, jugular venous disten- major defects that cannot be occluded readily by dressing technique
tion, decreased air entry, and hyperresonance on the affected side and,
sometimes, a clinically detectable shift of the trachea to the opposite side
with hypotension.
The treatment is immediate decompression of the pleural space,
which is accomplished initially by inserting a large-bore needle into
the pleural space at the second intercostal space in the midclavicular Chest wall
line or the fourth to fifth intercostal space just anterior to the midaxil-
lary line. If a plunger syringe is used with the needle, an immediate
spontaneous rise of the plunger in the barrel will be seen. This pro-
cedure should be followed by formal insertion of a chest tube. Briefly,
the technique of chest tube insertion requires an incision down to
the pleura in the fourth to fifth intercostal space just anterior to the Needle
midaxillary line. The large-bore chest tube (F32-F36) is inserted
directly with a clamp after verification by finger palpation that the
pleural space has been entered and there are no pleural adhesions
(Fig. 120-2). When needle decompression is performed and the chest
tube is not immediately available, the needle may be inserted through
the finger portion of a glove so that air may exit but not enter the Portion
pleural space from the atmosphere (Fig. 120-3). Once the chest tube is of glove
inserted, it is connected to an underwater seal system with the option
of applying suction.
In many trauma centers, immediate availability of the chest tube and
suction device allows chest tube decompression without prior needle FIGURE 120-3. Needle decompression of the pleural space. Use of the finger portion of
decompression in experienced hands. a glove prevents air from entering the pleural space.
section10.indd 1154 1/20/2015 9:21:02 AM