Page 276 - fbkCardioDiabetes_2017
P. 276
252 Cardio Diabetes Medicine 2017
In an analysis of 3,115 patients presenting with STEMI
who underwent primary PCI, High-grade atrioventricu-
lar block (HAVB) (second-degree Mobitz II or third-de-
gree atrioventricular block) was present at baseline in
46 patients (1.5%). Diabetes mellitus was one of the
independent predictors of HAVB. Mortality rate was
significantly higher in patients with versus without
HAVB at 1-, and 3-year follow-ups . The greater risk
22
of AV blocks in diabetics in setting of STEMI could
be due to dysautonomic disturbances of the disease
or the deleterious effects of hyperglycemia on the
conduction system.
Most of the elderly patients have many underlying
systemic diseases and multiple coronary risk fac-
tors. In a paper studying the prevalence of diabetes
in elderly patients requiring permanent cardiac pace-
maker insertion, there were more number of diabetic
population (11.1%). DM conferred an excessive risk of
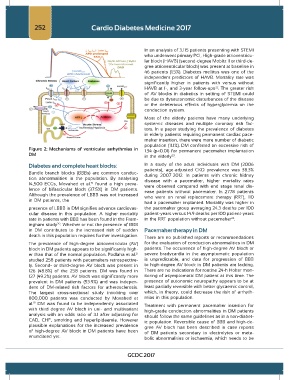
Figure 2: Mechanisms of ventricular arrhythmias in 1.34 (p<0.01) for permanent pacemaker implantation
DM in the elderly .
23
Diabetes and complete heart blocks: In a study of the adult individuals with DM (2006
Bundle branch blocks (BBBs) are common conduc- patients), age-adjusted CKD prevalence was 38.3%
during 2007–2012. In patients with chronic kidney
tion abnormalities in the population. By analysing disease with a pacemaker, higher mortality rates
14,500 ECGs, Movahed et al. found a high preva- were observed compared with end stage renal dis-
19
lence of bifascicular block (37.5%) in DM patients. ease patients without pacemaker. In 2778 patients
Although the prevalence of LBBB was not increased who were on renal replacement therapy (RRT), 110
in DM patients, the
had a pacemaker implanted. Mortality was higher in
presence of LBBB in DM signifies advance cardiovas- the pacemaker group averaging 24.3 deaths per 100
cular disease in this population. A higher mortality patient-years versus 14.9 deaths per 100 patient-years
24
rate in patients with BBB has been found in the Fram- in the RRT population without pacemaker .
ingham study . Whether or not the presence of BBB
20
in DM contributes to the increased risk of sudden Pacemaker therapy in DM
death in this population requires further investigation. There are no published reports or recommendations
The prevalence of high-degree atrioventricular (AV) for the evaluation of conduction abnormalities in DM
block in DM patients appears to be significantly high- patients. The occurrence of high-degree AV block or
er than that of the normal population. Podlaha et al. severe bradycardia in the asymptomatic population
21
studied 258 patients with pacemakers retrospective- is unpredictable, and data for progression of BBB
ly. Second- or third-degree AV block was present in to high-degree AV block in DM patients are lacking.
126 (48.8%) of the 258 patients. DM was found in There are no indications for routine 24-h Holter mon-
127 (49.2%) patients. AV block was significantly more itoring of asymptomatic DM patient at this time. The
prevalent in DM patients (53.9%) and was indepen- presence of autonomic neuropathy appears to be at
dent of DM-related risk factors for atherosclerosis. least partially reversible with better glycaemic control,
The largest cross-sectional study involving over which, in theory, could decrease the risk of arrhyth-
800,000 patients was conducted by Movahed et mias in this population.
19
al. DM was found to be independently associated Treatment with permanent pacemaker insertion for
with third degree AV block in uni- and multivariant high-grade conduction abnormalities in DM patients
analysis with an odds ratio of 3.1 after adjusting for should follow the same guidelines as in a non-diabet-
CAD, CHF, smoking and hyperlipidaemia. However ic population. Reversible cause of BBB and high-de-
plausible explanations for the increased prevalence gree AV block has been described in case reports
of high-degree AV block in DM patients have been of DM patients secondary to electrolytes or meta-
enunciated yet. bolic abnormalities or ischaemia, which needs to be
GCDC 2017