Page 868 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 868
CHAPTER 67: Endocarditis and Other Intravascular Infections 599
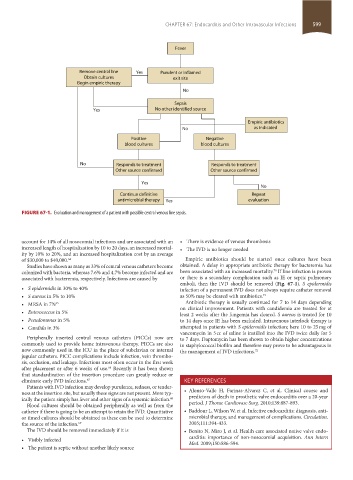
Fever
Remove central line Yes Purulent or inflamed
Obtain cultures exit site
Begin empiric therapy
No
Sepsis
Yes No other identified source
Empiric antibiotics
No as indicated
Positive Negative
blood cultures blood cultures
No Responds to treatment Responds to treatment
Other source confirmed Other source confirmed
Yes
No
Continue definitive Repeat
antimicrobial therapy Yes evaluation
FIGURE 67-1. Evaluation and management of a patient with possible central venous line sepsis.
account for 14% of all nosocomial infections and are associated with an • There is evidence of venous thrombosis
increased length of hospitalization by 10 to 20 days, an increased mortal- • The IVD is no longer needed
ity by 10% to 20%, and an increased hospitalization cost by an average
of $30,000 to $40,000. 64 Empiric antibiotics should be started once cultures have been
Studies have shown as many as 33% of central venous catheters become obtained. A delay in appropriate antibiotic therapy for bacteremia has
70
colonized with bacteria, whereas 7.6% and 4.7% become infected and are been associated with an increased mortality. If line infection is proven
associated with bacteremia, respectively. Infections are caused by or there is a secondary complication such as IE or septic pulmonary
emboli, then the IVD should be removed (Fig. 67-1). S epidermidis
• S epidermidis in 30% to 40% infection of a permanent IVD does not always require catheter removal
• S aureus in 5% to 10% as 50% may be cleared with antibiotics. 71
Antibiotic therapy is usually continued for 7 to 14 days depending
• MRSA in 7% 65 on clinical improvement. Patients with candidemia are treated for at
• Enterococcus in 5% least 2 weeks after the fungemia has cleared. S aureus is treated for 10
• Pseudomonas in 5% to 14 days once IE has been excluded. Intravenous interlock therapy is
• Candida in 3% attempted in patients with S epidermidis infection; here 10 to 25 mg of
vancomycin in 5 cc of saline is instilled into the IVD twice daily for 5
Peripherally inserted central venous catheters (PICCs) now are to 7 days. Daptomycin has been shown to obtain higher concentrations
commonly used to provide home intravenous therapy. PICCs are also in staphylococcal biofilm and therefore may prove to be advantageous in
now commonly used in the ICU in the place of subclavian or internal the management of IVD infections. 72
jugular catheters. PICC complications include infection, vein thrombo-
sis, occlusion, and leakage. Infections most often occur in the first week
after placement or after 6 weeks of use. Recently it has been shown
66
that standardization of the insertion procedure can greatly reduce or
eliminate early IVD infections. 67 KEY REFERENCES
Patients with IVD infection may develop purulence, redness, or tender-
ness at the insertion site, but usually these signs are not present. More typ- • Alonso-Valle H, Farinas-Alvarez C, et al. Clinical course and
ically the patient simply has fever and other signs of a systemic infection. 68 predictors of death in prosthetic valve endocarditis over a 20-year
Blood cultures should be obtained peripherally as well as from the period. J Thorac Cardiovasc Surg. 2010;139:887-893.
catheter if there is going to be an attempt to retain the IVD. Quantitative • Baddour L, Wilson W, et al. Infective endocarditis: diagnosis, anti-
or timed cultures should be obtained as these can be used to determine microbial therapy, and management of complications. Circulation.
the source of the infection. 69 2005;111:394-433.
The IVD should be removed immediately if it is • Benito N, Miro J, et al. Health care associated native valve endo-
• Visibly infected carditis: importance of non-nosocomial acquisition. Ann Intern
Med. 2009;150:586-594.
• The patient is septic without another likely source
section05_c61-73.indd 599 1/23/2015 12:48:02 PM