Page 947 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 947
678 PART 5: Infectious Disorders
Dura Pia
Brain abscess
Osteomyelitis
Diploic veins Epidural abscess
Subdural empyema
Frontal sinus
Arachnoid meningitis
Ethmoid air cells Cavernous sinus
thrombosis
Sphenoid sinus
Maxillary sinus Pituitary Optic N.
Cavernous
Int. Carotid A. sinus
III
V 1
V 2 IV
V 3 VI
Sphenoid Intersphenoid
sinuses septum
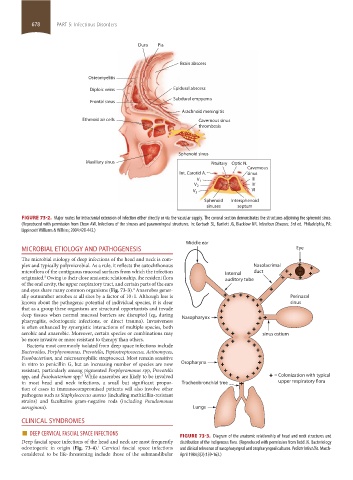
FIGURE 73-2. Major routes for intracranial extension of infection either directly or via the vascular supply. The coronal section demonstrates the structures adjoining the sphenoid sinus.
(Reproduced with permission from Chow AW. Infections of the sinuses and parameningeal structures. In: Gorbach SL, Bartlett JG, Blacklow NR. Infectious Diseases. 3rd ed. Philadelphia, PA:
Lippincott Williams & Wilkins; 2004:428-443.)
Middle ear
MICROBIAL ETIOLOGY AND PATHOGENESIS Eye
The microbial etiology of deep infections of the head and neck is com-
plex and typically polymicrobial. As a rule, it reflects the autochthonous Nasolacrimal
microflora of the contiguous mucosal surfaces from which the infection Internal duct
originated. Owing to their close anatomic relationship, the resident flora auditory tube
3
of the oral cavity, the upper respiratory tract, and certain parts of the ears
and eyes share many common organisms (Fig. 73-3). Anaerobes gener-
4
ally outnumber aerobes at all sites by a factor of 10 : 1. Although less is Perinasal
known about the pathogenic potential of individual species, it is clear sinus
that as a group these organisms are structural opportunists and invade
deep tissues when normal mucosal barriers are disrupted (eg, during Nasopharynx
pharyngitis, odontogenic infections, or direct trauma). Invasiveness
is often enhanced by synergistic interactions of multiple species, both
aerobic and anaerobic. Moreover, certain species or combinations may sinus ostium
be more invasive or more resistant to therapy than others.
Bacteria most commonly isolated from deep space infections include
Bacteroides, Porphyromonas, Prevotella, Peptostreptococcus, Actinomyces,
Fusobacterium, and microaerophilic streptococci. Most remain sensitive
in vitro to penicillin G, but an increasing number of species are now Oropharynx
resistant, particularly among pigmented Porphyromonas spp, Prevotella
spp, and Fusobacterium spp. While anaerobes are likely to be involved = Colonization with typical
5
in most head and neck infections, a small but significant propor- Tracheobronchial tree upper respiratory flora
tion of cases in immunocompromised patients will also involve other
pathogens such as Staphylococcus aureus (including methicillin-resistant
strains) and facultative gram-negative rods (including Pseudomonas
aeruginosa). Lungs
CLINICAL SYNDROMES
■ DEEP CERVICAL FASCIAL SPACE INFECTIONS
Deep fascial space infections of the head and neck are most frequently FIGURE 73-3. Diagram of the anatomic relationship of head and neck structures and
distribution of the indigenous flora. (Reproduced with permission from Todd JK. Bacteriology
odontogenic in origin (Fig. 73-4). Cervical fascial space infections and clinical relevance of nasopharyngeal and oropharyngeal cultures. Pediatr Infect Dis. March-
1
considered to be life-threatening include those of the submandibular April 1984;3(2):159-163.)
section05_c61-73.indd 678 1/23/2015 12:48:56 PM