Page 425 - Cardiac Nursing
P. 425
/09
/30
P
:57
6
0-4
p40
qxd
19.
pta
1 A
Inc
ra
40
P
M
a
a
LWBK340-c18_p400-419.qxd 6/30/09 7:57 PM Page 401 Aptara Inc.
LWB
LWB K34 0-c 18_ p40 0-4 19. qxd 6 /30 /09 7 7 :57 P M P a g g e e 40 1 A pta ra Inc . .
18_
0-c
K34
C HAPTER 1 8 / Cardiac Electrophysiology Procedures 401
Superior Aorta
Vena Cava (SVC)
Pulmonary artery
His bundle
catheter
High right atrial
catheter
Left pulmonary
veins
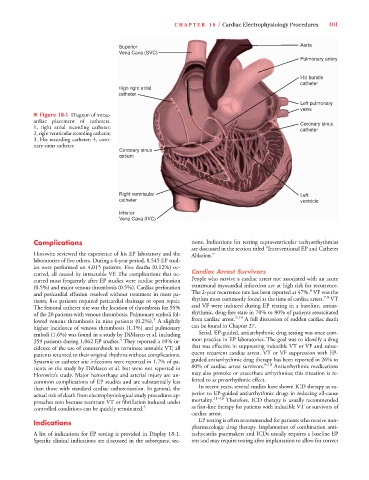
■ Figure 18-1 Diagram of intrac-
ardiac placement of catheters. Coronary sinus
1, right atrial recording catheter; catheter
2, right ventricular recording catheter;
3, His recording catheter; 4, coro-
nary sinus catheter.
Coronary sinus
ostium
Right ventricular Left
catheter ventricle
Inferior
Vena Cava (IVC)
Complications tions. Indications for testing supraventricular tachyarrhythmias
are discussed in the section titled “Interventional EP and Catheter
Horowitz reviewed the experience of his EP laboratory and the Ablation.”
laboratories of five others. During a 4-year period, 8,545 EP stud-
ies were performed on 4,015 patients. Five deaths (0.12%) oc-
curred, all caused by intractable VF. The complications that oc- Cardiac Arrest Survivors
curred most frequently after EP studies were cardiac perforation People who survive a cardiac arrest not associated with an acute
(0.5%) and major venous thrombosis (0.5%). Cardiac perforation transmural myocardial infarction are at high risk for recurrence.
6
and pericardial effusion resolved without treatment in most pa- The 2-year recurrence rate has been reported at 47%. VF was the
7,8
tients; five patients required pericardial drainage or open repair. rhythm most commonly found at the time of cardiac arrest. VT
The femoral catheter site was the location of thrombosis for 95% and VF were induced during EP testing in a baseline, antiar-
of the 20 patients with venous thrombosis. Pulmonary emboli fol- rhythmic, drug-free state in 70% to 80% of patients resuscitated
9,10
1
lowed venous thrombosis in nine patients (0.2%). A slightly from cardiac arrest. A full discussion of sudden cardiac death
higher incidence of venous thrombosis (1.1%) and pulmonary can be found in Chapter 27.
emboli (1.6%) was found in a study by DiMarco et al. including Serial, EP-guided, antiarrhythmic drug testing was once com-
4
359 patients during 1,062 EP studies. They reported a 10% in- mon practice in EP laboratories. The goal was to identify a drug
cidence of the use of countershock to terminate unstable VT; all that was effective in suppressing inducible VT or VF and subse-
patients returned to their original rhythms without complications. quent recurrent cardiac arrest. VT or VF suppression with EP-
Systemic or catheter site infections were reported in 1.7% of pa- guided antiarrhythmic drug therapy has been reported in 26% to
9,10
tients in the study by DiMarco et al. but were not reported in 80% of cardiac arrest survivors. Antiarrhythmic medications
Horowitz’s study. Major hemorrhage and arterial injury are un- may also provoke or exacerbate arrhythmias; this situation is re-
common complications of EP studies and are substantially less ferred to as proarrhythmic effect.
than those with standard cardiac catheterization. In general, the In recent years, several studies have shown ICD therapy as su-
actual risk of death from electrophysiological study procedures ap- perior to EP-guided antiarrhythmic drugs in reducing all-cause
11–16
proaches zero because reentrant VT or fibrillation induced under mortality. Therefore, ICD therapy is usually recommended
controlled conditions can be quickly terminated. 5 as first-line therapy for patients with inducible VT or survivors of
cardiac arrest.
Indications EP testing is often recommended for patients who receive non-
pharmacologic drug therapy. Implantation of combination anti-
A list of indications for EP testing is provided in Display 18-1. tachycardia pacemakers and ICDs usually requires a baseline EP
Specific clinical indications are discussed in the subsequent sec- test and may require testing after implantation to allow for correct