Page 663 - Cardiac Nursing
P. 663
p
63
p
Pa
Pa
63
8-6
54.
8-6
Pa
M
39
39
A
p
A
39
g
g
g
e 6
e 6
1
1
/09
/09
/09
1
1 A
M
1 A
2:0
2:0
q
q
q
54.
54.
xd
/30
/30
6
xd
6
p
LWB K34 0-c 27_ pp638-654.qxd 6/30/09 12:01 AM Page 639 Aptara Inc.
LWB
c.
c.
LWBK340-c27_
27_
0-c
K34
27_
ara
a
a
ara
t
t
p
In
In
C HAPTER 2 7 / Sudden Cardiac Death and Cardiac Arrest 639
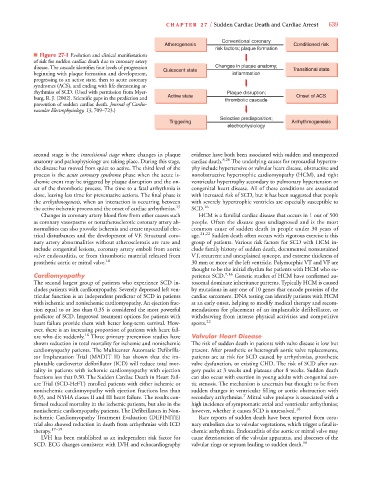
Conventional coronary
Atherogenesis Conditioned risk
risk factors; plaque formation
■ Figure 27-1 Evolution and clinical manifestations
of risk for sudden cardiac death due to coronary artery
disease. The cascade identifies four levels of progression Quiescent state Changes in plaque anatomy; Transitional state
beginning with plaque formation and development, inflammation
progressing to an active state, then to acute coronary
syndromes (ACS), and ending with life-threatening ar-
rhythmias of SCD. (Used with permission from Myer- Plaque disruption;
burg, R. J. [2002]. Scientific gaps in the prediction and Active state thrombotic cascade Onset of ACS
prevention of sudden cardiac death. Journal of Cardio-
vascular Electrophysiology, 13, 709–723.)
Selective predisposition;
Triggering Arrhythmogenesis
electrophysiology
second stage is the transitional stage where changes in plaque evidence have both been associated with sudden and unexpected
anatomy and pathophysiology are taking place. During this stage, cardiac death. 8,20 The underlying causes for myocardial hypertro-
the disease has moved from quiet to active. The third level of the phy include hypertensive or valvular heart disease, obstructive and
process is the acute coronary syndrome phase when the acute is- nonobstructive hypertrophic cardiomyopathy (HCM), and right
chemic event may be triggered by plaque disruption and the on- ventricular hypertrophy secondary to pulmonary hypertension or
set of the thrombotic process. The time to a fatal arrhythmia is congenital heart disease. All of these conditions are associated
close, leaving less time for preventative actions. The final phase is with increased risk of SCD, but it has been suggested that people
the arrhythmogenesis, when an interaction is occurring between with severely hypertrophic ventricles are especially susceptible to
the active ischemic process and the onset of cardiac arrhythmias. 15 SCD. 16
Changes in coronary artery blood flow from other causes such HCM is a familial cardiac disease that occurs in 1 out of 500
as coronary vasospasms or nonatherosclerotic coronary artery ab- people. Often the disease goes undiagnosed and is the most
normalities can also provoke ischemia and create myocardial elec- common cause of sudden death in people under 30 years of
trical disturbances and the development of VF. Structural coro- age. 21,22 Sudden death often occurs with vigorous exercise is this
nary artery abnormalities without atherosclerosis are rare and group of patients. Various risk factors for SCD with HCM in-
include congenital lesions, coronary artery emboli from aortic clude family history of sudden death, documented nonsustained
valve endocarditis, or from thrombotic material released from VT, recurrent and unexplained syncope, and extreme thickness of
prosthetic aortic or mitral valve. 16 30 mm or more of the left ventricle. Polymorphic VT and VF are
thought to be the initial rhythm for patients with HCM who ex-
Cardiomyopathy perience SCD. 7,16 Genetic studies of HCM have confirmed au-
The second largest group of patients who experience SCD in- tosomal dominate inheritance patterns. Typically HCM is caused
cludes patients with cardiomyopathy. Severely depressed left ven- by mutations in any one of 10 genes that encode proteins of the
tricular function is an independent predictor of SCD in patients cardiac sarcomere. DNA testing can identify patients with HCM
with ischemic and nonischemic cardiomyopathy. An ejection frac- at an early onset, helping to modify medical therapy and recom-
tion equal to or less than 0.35 is considered the most powerful mendations for placement of an implantable defibrillator, or
predictor of SCD. Improved treatment options for patients with withdrawing from intense physical activities and competitive
heart failure provide them with better long-term survival. How- sports. 22
ever, there is an increasing proportion of patients with heart fail-
ure who die suddenly. 16 Three primary prevention studies have Valvular Heart Disease
shown reduction in total mortality for ischemic and nonischemic The risk of sudden death in patients with valve disease is low but
cardiomyopathy patients. The Multicenter Automatic Defibrilla- present. After prosthetic or heterograft aortic valve replacements,
tor Implantation Trial (MADIT II) has shown that the im- patients are at risk for SCD caused by arrhythmias, prosthetic
plantable cardioverter defibrillator (ICD) will reduce total mor- valve dysfunction, or existing CHD. The risk of SCD after sur-
tality in patients with ischemic cardiomyopathy with ejection gery peaks at 3 weeks and plateaus after 8 weeks. Sudden death
fractions less that 0.30. The Sudden Cardiac Death in Heart Fail- can also occur with exertion in young adults with congenital aor-
ure Trial (SCD-HeFT) enrolled patients with either ischemic or tic stenosis. The mechanism is uncertain but thought to be from
nonischemic cardiomyopathy with ejection fractions less than sudden changes in ventricular filling or aortic obstruction with
7
0.35, and NYHA classes II and III heart failure. The results con- secondary arrhythmias. Mitral valve prolapse is associated with a
firmed reduced mortality in the ischemic patients, but also in the high incidence of symptomatic atrial and ventricular arrhythmias;
nonischemic cardiomyopathy patients. The Defibrillators in Non- however, whether it causes SCD is unresolved. 16
ischemic Cardiomyopathy Treatment Evaluation (DEFINITE) Rare reports of sudden death have been reported from coro-
trial also showed reduction in death from arrhythmias with ICD nary embolism due to valvular vegetations, which trigger a fatal is-
therapy. 17–19 chemic arrhythmia. Endocarditis of the aortic or mitral valve may
LVH has been established as an independent risk factor for cause deterioration of the valvular apparatus, and abscesses of the
SCD. ECG changes consistent with LVH and echocardiography valvular rings or septum leading to sudden death. 16