Page 464 - ACCCN's Critical Care Nursing
P. 464
Neurological Assessment and Monitoring 441
Case study, Continued
Emergency surgery noradrenaline support for a CPP of 65; SaO 2 97%; temperature
Due to his continued bilateral pupil enlargement and non reac- 35.5°C; his pupils returning to a stabilised 3/3 mm (R/L), sluggish
tivity, Daniel was transferred to the operating theatre within the sequential reaction; he was heavily sedated, not paralysed initially,
hour for a craniotomy and insertion of external ventricular drain and unresponsive with a Glasgow Coma Scale score (GCS) of 3T
(EVD) and evacuation of the subdural haematoma. A repeat CT (eye opening 1, verbal 1 [T = intubated], motor 1). The initial
scan revealed reduced cerebral oedema and repositioning of the opening intracranial pressure of 28 mmHg was indicative of the
ventricular midline shift. Widespread petechial hemorrhages cerebral oedema from the diffuse injury. The EVD was positioned
remained. In terms of his further injuries, a right femur external at 15 cm above the tragus and remained opened during episodes
fixation, right femoral artery repair, lateral right thigh fasciotomy, of increased ICP exceeding 20 mmHg and drained 26 mL of blood-
and right forearm fracture stabilisation by plaster cast were per- tinged cerebral spinal fluid in the first 24 hours. He required para-
formed in conjunction with his neurosurgery due to a large lysing and increased sedation to control his ICP and CPP. Pain
amount of blood loss mainly from the right femur. The right peri- stimulation for neurological assessment under these conditions
nephric haematoma had stabilised and was managed conserva- was only assessed during endotracheal suction. Noradrenaline
tively. A left subclavian central venous catheter was placed and a infusion fluctuated throughout the day and Daniel required hypo-
radial arterial cannulation for arterial blood pressure monitoring. tonic saline boluses for intracranial hypertension. Normal saline
was infused to maintain euovolemia.
Daniel received a massive blood transfusion:
● 34 units packed red blood cells Days 2–7
● 17 units fresh frozen plasma Daniel’s clinical parameters and assessment are shown in Table
● 10 units cryoprecipitate 16.10. His condition remained variable and on days 3 and 4 his
● 5 units platelets ICP and CPP were unstable with increasing need for sedation and
● 7 L voluven (hydroxyethyl starch/normal saline) paralysis. His pupils enlarged to size 5 and became unreactive.
● 4.5 L Hartmans solution He was stabilised with boluses of hypertonic saline and increased
● 2.5 L normal saline drainage from the EVD which totalled 35 mL for the day. A repeat
CT determined a diffuse injury with global cerebral oedema. The
Following surgery, he was admitted to the Intensive Care Unit (ICU) ventricles were effaced but not compressed. After stabilising on
for further management day 4, Daniel’s sedation was turned off the morning of day 5 for
ICU management neurological assessment. His GCS was 5 (E2 V1(T)M3) with normal
Day 1 flexion to pain and remained unchanged until day 7. His GCS
On arrival to the ICU, Daniel’s condition was critical but stable: may have increased but it was difficult to assess his verbal response
heart rate = 132 beats/min; intubated and ventilated at 14 breaths/ whilst intubated. The EVD was removed on day 6 and he remained
min, Vt 500 mL, FiO 2 = 0.7, Positive End Expiratory Pressure sedated and ventilated to support his chest injuries. Daniel con-
(PEEP) = 10 cmH 2 O; blood pressure 160/65 mmHg (MAP 93) with tinued to slowly recover.
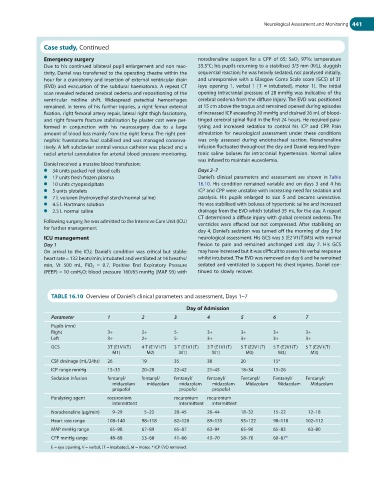
TABLE 16.10 Overview of Daniel’s clinical parameters and assessment, Days 1–7
Day of Admission
Parameter 1 2 3 4 5 6 7
Pupils (mm)
Right 3+ 2+ 5- 3+ 3+ 3+ 3+
Left 3+ 2+ 5- 3+ 3+ 3+ 3+
GCS 3T (E1V1(T) 4 T (E1V1(T) 3 T (E1V1(T) 3 T (E1V1(T) 5 T (E2V1(T) 5 T (E2V1(T) 5 T (E2V1(T)
M1) M2) M1) M1) M3) M3) M3)
CSF drainage (mL/24hr) 26 19 35 38 20 15*
ICP range mmHg 15–35 20–28 22–42 21–45 18–34 15–26
Sedation infusion fentanyl/ fentanyl/ fentanyl/ fentanyl/ Fentanyl/ Fentanyl/ Fentanyl/
midazolam midazolam midazolam midazolam Midazolam Midazolam Midazolam
propofol propofol propofol
Paralysing agent rocuronium rocuronium rocuronium
intermittent intermittent intermittent
Noradrenaline (µg/min) 9–29 5–22 28–45 26–44 18–32 15–22 12–18
Heart rate range 108–140 98–118 82–128 89–135 95–122 98–118 102–112
MAP mmHg range 65–98 67–89 65–87 63–94 65–90 65–83 63–80
CPP mmHg range 48–68 53–68 41–66 43–70 58–70 60–67*
E = eye opening, V = verbal, [T = intubated], M = motor, * ICP EVD removed.